
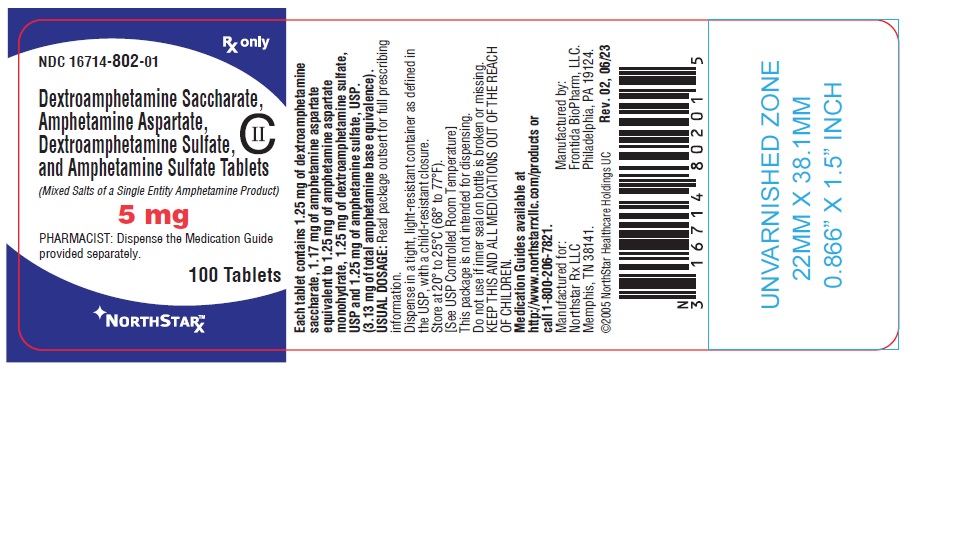
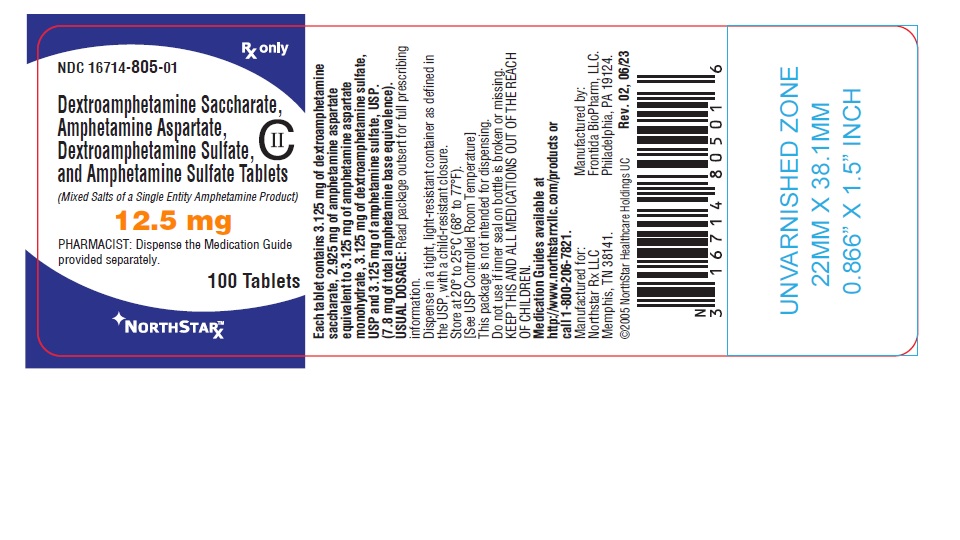
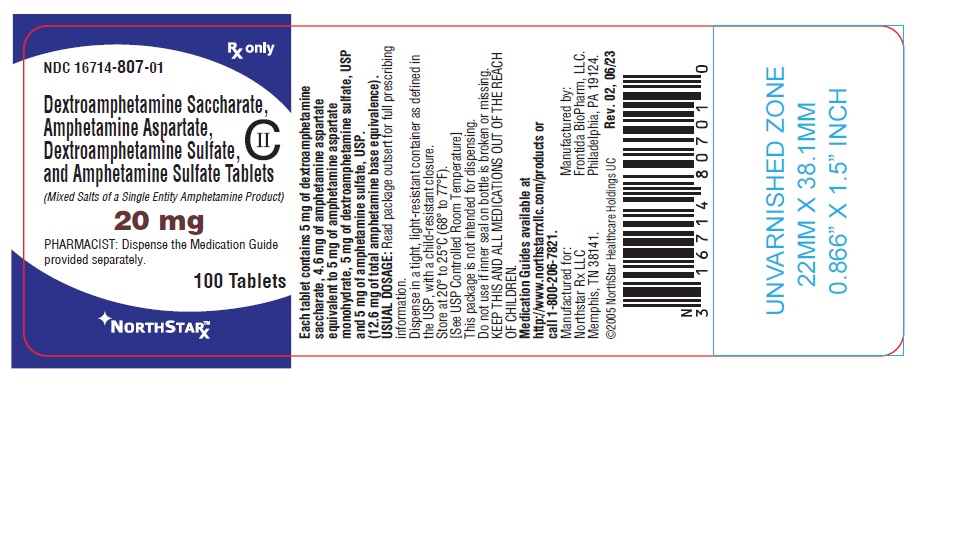
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate while Breastfeeding
What is Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate ?
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate safe in breastfeeding?

Usage in Nursing Mothers Amphetamines are excreted in human milk. Mothers taking amphetamines should be advised to refrain from nursing.
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate Breastfeeding Analsys
Dextroamphetamine saccharate while Breastfeeding
Low RiskCAS Number: 51-63-8
A sympathomimetic drug and central nervous system stimulant, it has a similar action and uses to amphetamine, its dextro isomer.It is used (GSK, 2007) in the treatment of narcolepsy (Wise, 2007) and Attention Deficit Hyperactivity Disorder (ADHD), and is also used as an illegal drug (Oei, 2012). It is excreted in breast milk, concentrating about 3 times more than in plasma. This concentration assumes a relative dose about 6% (Ilett, 2007). In infants whose mothers were taking dexamfetamine as treatment for ADHD, levels ranging from undetectable to 14% of maternal plasma levels have been measured and no problems were observed in the clinical follow-up of these infants (Ilett, 2007). There is little information on the impact of amphetamine abuse on the development and health of infants (Oei, 2012, Wise, 2007; Moretti, 2000), but it is known that they are more exposed to social problems, domestic violence, and lower breastfeeding rates (Oei, 2010). There is controversy over the possibly mild negative effect of amphetamine on prolactin (Petraglia, 1987; DeLeo, 1983), but milk production in mothers who took it therapeutically was not affected (Öhman, 2015). During breastfeeding, the therapeutic use (narcolepsy, ADHD) of dexamphetamine can be assessed, using the lowest possible effective dose and monitoring the occurrence of irritability, insomnia, lack of appetite and weight loss. Its use as an illegal drug is totally discouraged (Oei, 2012). See below the information of these related products:
Amphetamine aspartate while Breastfeeding
UnsafeCAS Number: 300-62-9

A sympathomimetic drug and central nervous system stimulant, it has a similar action and uses to its isomer dextroamphetamine.It is used in the treatment of narcolepsy (Wise, 2007) and Attention Deficit Hyperactivity Disorder (ADHD), and is also used as an illegal drug (Oei, 2012; Bartu, 2009). It is excreted in breast milk, concentrating between 2 and 8 times more than in plasma (FDA, 2017; Steiner, 1984). This concentration, although it could be significant (Bartu, 2009), assumes a relative dose between 2% (Öhman, 2015) and 13.8% (FDA, 2017). In infants whose mothers were taking amphetamine as narcolepsy treatment, low plasma levels (Öhman, 2015) and urine (Steiner, 1984) were measured and no problems were observed in the clinical follow-up of these infants (Öhman, 2015; Steiner, 1984). There is little information on the impact of amphetamine abuse on the development and health of infants (Oei, 2012, Wise, 2007; Moretti, 2000), but it is known that they are more exposed to social problems, domestic violence, and lower breastfeeding rates (Oei, 2010). To minimize the risk, it is estimated that 48 hours should pass after the last amphetamine-based recreational use, before breast-feeding (Bartu, 2009). There is controversy over the possibly mild negative effect of amphetamine on prolactin (Petraglia, 1987; DeLeo, 1983), but milk production in mothers who took it therapeutically was not affected (Öhman, 2015). During breastfeeding, the therapeutic use (narcolepsy, ADHD) of amphetamine can be assessed, using the lowest possible effective dose and monitoring the occurrence of irritability, insomnia, lack of appetite and weight loss. Its use as an illegal drug is totally discouraged (Oei, 2012).
Dextroamphetamine sulfate while Breastfeeding
Low RiskCAS Number: 51-63-8

A sympathomimetic drug and central nervous system stimulant, it has a similar action and uses to amphetamine, its dextro isomer.It is used (GSK, 2007) in the treatment of narcolepsy (Wise, 2007) and Attention Deficit Hyperactivity Disorder (ADHD), and is also used as an illegal drug (Oei, 2012). It is excreted in breast milk, concentrating about 3 times more than in plasma. This concentration assumes a relative dose about 6% (Ilett, 2007). In infants whose mothers were taking dexamfetamine as treatment for ADHD, levels ranging from undetectable to 14% of maternal plasma levels have been measured and no problems were observed in the clinical follow-up of these infants (Ilett, 2007). There is little information on the impact of amphetamine abuse on the development and health of infants (Oei, 2012, Wise, 2007; Moretti, 2000), but it is known that they are more exposed to social problems, domestic violence, and lower breastfeeding rates (Oei, 2010). There is controversy over the possibly mild negative effect of amphetamine on prolactin (Petraglia, 1987; DeLeo, 1983), but milk production in mothers who took it therapeutically was not affected (Öhman, 2015). During breastfeeding, the therapeutic use (narcolepsy, ADHD) of dexamphetamine can be assessed, using the lowest possible effective dose and monitoring the occurrence of irritability, insomnia, lack of appetite and weight loss. Its use as an illegal drug is totally discouraged (Oei, 2012). See below the information of these related products:
Amphetamine sulfate while Breastfeeding
UnsafeCAS Number: 300-62-9
A sympathomimetic drug and central nervous system stimulant, it has a similar action and uses to its isomer dextroamphetamine.It is used in the treatment of narcolepsy (Wise, 2007) and Attention Deficit Hyperactivity Disorder (ADHD), and is also used as an illegal drug (Oei, 2012; Bartu, 2009). It is excreted in breast milk, concentrating between 2 and 8 times more than in plasma (FDA, 2017; Steiner, 1984). This concentration, although it could be significant (Bartu, 2009), assumes a relative dose between 2% (Öhman, 2015) and 13.8% (FDA, 2017). In infants whose mothers were taking amphetamine as narcolepsy treatment, low plasma levels (Öhman, 2015) and urine (Steiner, 1984) were measured and no problems were observed in the clinical follow-up of these infants (Öhman, 2015; Steiner, 1984). There is little information on the impact of amphetamine abuse on the development and health of infants (Oei, 2012, Wise, 2007; Moretti, 2000), but it is known that they are more exposed to social problems, domestic violence, and lower breastfeeding rates (Oei, 2010). To minimize the risk, it is estimated that 48 hours should pass after the last amphetamine-based recreational use, before breast-feeding (Bartu, 2009). There is controversy over the possibly mild negative effect of amphetamine on prolactin (Petraglia, 1987; DeLeo, 1983), but milk production in mothers who took it therapeutically was not affected (Öhman, 2015). During breastfeeding, the therapeutic use (narcolepsy, ADHD) of amphetamine can be assessed, using the lowest possible effective dose and monitoring the occurrence of irritability, insomnia, lack of appetite and weight loss. Its use as an illegal drug is totally discouraged (Oei, 2012).
Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate Breastfeeding Analsys - 2
Dextroamphetamine saccharate while Breastfeeding
CAS Number: 51-64-9
In dosages prescribed for medical indications, some evidence indicates that dextroamphetamine might not affect nursing infants adversely. The effect of dextroamphetamine in milk on the neurological development of the infant has not been well studied. It is possible that large dosages of dextroamphetamine might interfere with milk production, especially in women whose lactation is not well established. Relevant published information was not found as of the revision date on the safety of breastfeeding during amphetamine abuse. One expert recommends that amphetamines not be used therapeutically in nursing mothers.[1]
Amphetamine aspartate while Breastfeeding
CAS Number: 300-62-9
In dosages prescribed for medical indications, some evidence indicates that amphetamine does not affect nursing infants adversely. The effect of amphetamine in milk on the neurological development of the infant has not been well studied. Large dosages of amphetamine might interfere with milk production, especially in women whose lactation is not well established. Breastfeeding is generally discouraged in mothers who are actively abusing amphetamines.[1][2][3] One expert recommends that amphetamine not be used therapeutically in nursing mothers.[4]
Dextroamphetamine sulfate while Breastfeeding
CAS Number: 51-64-9

In dosages prescribed for medical indications, some evidence indicates that dextroamphetamine might not affect nursing infants adversely. The effect of dextroamphetamine in milk on the neurological development of the infant has not been well studied. It is possible that large dosages of dextroamphetamine might interfere with milk production, especially in women whose lactation is not well established. Relevant published information was not found as of the revision date on the safety of breastfeeding during amphetamine abuse. One expert recommends that amphetamines not be used therapeutically in nursing mothers.[1]
Amphetamine sulfate while Breastfeeding
CAS Number: 300-62-9
In dosages prescribed for medical indications, some evidence indicates that amphetamine does not affect nursing infants adversely. The effect of amphetamine in milk on the neurological development of the infant has not been well studied. Large dosages of amphetamine might interfere with milk production, especially in women whose lactation is not well established. Breastfeeding is generally discouraged in mothers who are actively abusing amphetamines.[1][2][3] One expert recommends that amphetamine not be used therapeutically in nursing mothers.[4]
What should I do if already breastfed my kid after using Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate?
We have already established that Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate is unsafe in breastfeeding and breastfeeding while using Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate is not a good idea however if have already used
My doctor has prescribed me Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate, what should I do?
If your doctor knows that you are breastfeeding mother and still prescribes Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate then there must be good reason for that as Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate is considered unsafe, It usually happens when doctor finds that overall advantage of taking
If I am using Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate, will my baby need extra monitoring?
Yes, Extra monitoring is required if mother is using Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate and breastfeeding as it is considered unsafe for baby.
Who can I talk to if I have questions about usage of Dextroamphetamine Saccharate, Amphetamine Aspartate, Dextroamphetamine Sulfate, And Amphetamine Sulfate in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
