Modern medicine has evolved so much so that sooner or later every breastfeeding mother needs to take it in one form or other. Medication that is present in mothers blood will transfer into her breast milk to some extent. Most drugs do so at low levels and pose no real risk to infants but then there are some exceptions. In This post will discuss whether Dopamine Hydrochloride Injection is safe in breast-feeding or not.
What is Dopamine Hydrochloride Injection used for?
Dopamine Hydrochloride, USP is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarction, trauma, endotoxic septicemia, open-heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure. Patients most likely to respond adequately to Dopamine Hydrochloride, USP are those in whom physiological parameters, such as urine flow, myocardial function, and blood pressure, have not undergone profound deterioration. Multiclinic trials indicate that the shorter the time interval between onset of signs and symptoms and initiation of therapy with blood volume correction and Dopamine Hydrochloride, USP, the better the prognosis. Where appropriate, blood volume restoration with a suitable plasma expander or whole blood should be accomplished prior to administration of Dopamine Hydrochloride, USP. Poor Perfusion of Vital Organs – Urine flow appears to be one of the better diagnostic signs by which adequacy of vital organ perfusion can be monitored. Nevertheless, the physician should also observe the patient for signs of reversal of confusion or reversal of comatose condition. Loss of pallor, increase in toe temperature, and/or adequacy of nail bed capillary filling may also be used as indices of adequate dosage. Clinical studies have shown that when Dopamine Hydrochloride, USP is administered before urine flow has diminished to levels of approximately 0.3 mL/minute, prognosis is more favorable. Nevertheless, in a number of oliguric or anuric patients, administration of Dopamine Hydrochloride, USP has resulted in an increase in urine flow, which in some cases reached normal levels. Dopamine Hydrochloride, USP may also increase urine flow in patients whose output is within normal limits and thus may be of value in reducing the degree of pre-existing fluid accumulation. It should be noted that at doses above those optimal for the individual patient, urine flow may decrease, necessitating reduction of dosage. Low Cardiac Output – Increased cardiac output is related to dopamine’s direct inotropic effect on the myocardium. Increased cardiac output at low or moderate doses appears to be related to a favorable prognosis. Increase in cardiac output has been associated with either static or decreased systemic vascular resistance (SVR). Static or decreased SVR associated with low or moderate movements in cardiac output is believed to be a reflection of differential effects on specific vascular beds with increased resistance in peripheral beds (e.g., femoral) and concomitant decreases in mesenteric and renal vascular beds. Redistribution of blood flow parallels these changes so that an increase in cardiac output is accompanied by an increase in mesenteric and renal blood flow. In many instances the renal fraction of the total cardiac output has been found to increase. Increase in cardiac output produced by dopamine is not associated with substantial decreases in systemic vascular resistance as may occur with isoproterenol. Hypotension – Hypotension due to inadequate cardiac output can be managed by administration of low to moderate doses of Dopamine Hydrochloride, USP which have little effect on SVR. At high therapeutic doses, dopamine’s alpha-adrenergic activity becomes more prominent and thus may correct hypotension due to diminished SVR. As in the case of other circulatory decompensation states, prognosis is better in patients whose blood pressure and urine flow have not undergone profound deterioration. Therefore, it is suggested that the physician administer Dopamine Hydrochloride, USP as soon as a definite trend toward decreased systolic and diastolic pressure becomes evident.
Dopamine Hydrochloride Injection while breastfeeding safe or not? Can there be any side effects for infant while using it during breastfeeding?
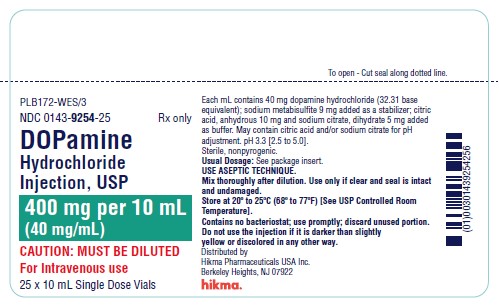
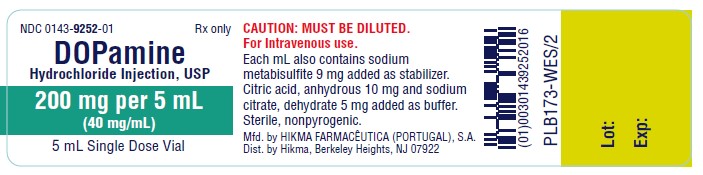
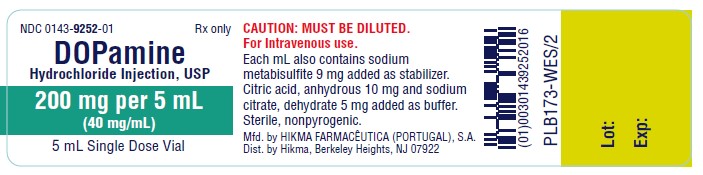
Dopamine hydrochloride is the one and only active ingredient present in Dopamine Hydrochloride Injection. Dopamine hydrochloride in itself is a low risk drug for lactation so it is easy to understand that Dopamine Hydrochloride Injection also comes in category of Low Risk item while breastfeeding. Below is the summary of Dopamine hydrochloride in breastfeeding.
Statement of Manufacturer/Labeler about breastfeeding usage
Nursing Mothers It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when dopamine HCl is administered to a nursing woman.
Dopamine Hydrochloride Injection Breastfeeding Analsys
Low RiskIt may inhibit lactation.
Dopamine Hydrochloride Injection Breastfeeding Analsys - 2
CAS Number: 51-61-6
No information is available on the use of dopamine during breastfeeding. Because of its poor oral bioavailability and short half-life, any dopamine in milk is unlikely to affect the infant. Intravenous dopamine infusion may decrease milk production. Dopamine is known to reduce serum prolactin in nonnursing women, but no information is available on its effect on milk production in nursing mothers.
I am nursing mother and I have already used Dopamine Hydrochloride Injection, what should I do?
During whole lactation period you shall first discuss with your doctor and then together you shall decide whether you shall take that drug or not however if you have already taken Dopamine Hydrochloride Injection then you shall inform your doctor, But you should not be worried too much as Dopamine Hydrochloride Injection comes in category of low risk drug.
I am nursing mother and my doctor has suggested me to use Dopamine Hydrochloride Injection, is it safe?
Though Dopamine Hydrochloride Injection dose not comes in category of safe drugs rather it comes in category of low risk but if your doctor is aware that you are breastfeeding your baby and has still recommended it then its advantages must be outweighing the risks.
If I am using Dopamine Hydrochloride Injection, will my baby need extra monitoring?
Not much
Who can I talk to if I have questions about usage of Dopamine Hydrochloride Injection in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
Drug Brands with same Active ingredients