Shingles while Breastfeeding
What is Shingles used for?
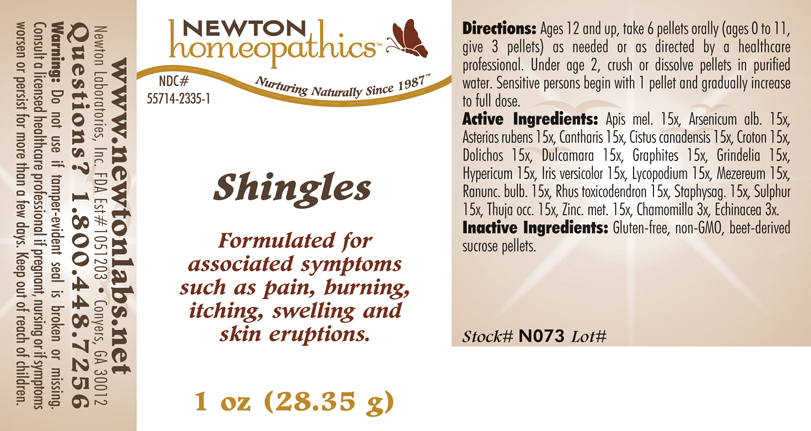
Purpose: OTC - PURPOSE SECTION Formulated for associated symptoms such as pain, burning, itching, swelling and skin eruptions.
Is Shingles usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Shingles Breastfeeding Analsys
Arsenic trioxide while Breastfeeding
DangerousUsed in the treatment of promyelocitic leukemia in adults.
Hypericum perforatum while Breastfeeding
SafeCAS Number: 68917-49-7
Herb commonly used from ancient times. Firm evidence is available on its effectiveness for treatment of depression, to the extent that it should be avoided a sudden stop of medication to prevent a rebound effect. It has been also topically used for the treatment of wounds, burns and eczema due to healing and antiseptical properties. Constituents are: Hypericin, Hyperforin and Quercetin. Antidepressant properties are attributed to Hypericin but mostly to Hyperforin. Quercetin is a flavonoid which is commonly found in many fruits and eatable vegetables. Hyperforin is excreted into breast milk in nil or clinically non-significant amount with not side-effects reported among breastfed infants from treated mothers, except for isolated and dubious cases of somnolence and colicky pain with spontaneous resolution with no medical intervention being required. Plasma levels in those infants were undetectable or close to the lower detectable point (0.1μg/L). Hypericin has not been detected in the breast milk. Quercetin levels found were as low as of few nanomols/L., and related to composition of fruits and vegetables of diet. It is most important to make sure that composition and amount of Hypericum contained in commercially available products is correct, do not take it without medical surveillance, avoid sudden stop and consider pharmacological interactions with many other medications.
Lycopodium clavatum spore while Breastfeeding
UnsafeAerial summits and spores of this fern are used. Traditionally use as a diuretic and intestinal spasm relief drug. Also used for abrasions and skin irritation. It may be a cause of asthma and contact dermatitis.
Zinc while Breastfeeding
SafeZinc (Zn) is an essential element for nutrition. It is present in many foods.Recommended daily allowance of Zn is 8 to 15 mg. (Moran Hall 2010). Millions of people worldwide are Zn-deficient.It is used as a treatment for Wilson's disease and Acrodermatitis Enteropathica. Zn is involved in the regulation process of lactation (Lee 2016).Pasteurization of the milk does not affect the concentration of Zn and other trace elements (Mohd Taufek-2016). The average concentration of Zn in breastmilk is 4 to 16 mg / L (Picciano 1976, Hannan 2005, Dórea 2012) which is independent of plasma levels and maternal daily intake (Krebs 1995, Chierici 1999, Hannan 2009).Intestinal absorption of zinc is almost doubled during pregnancy and lactation (Fung 1997).Zinc levels in the infant are dependent on Zinc levels in the breast milk (Dumrongwongsiri 2015)With a varied and balanced diet, an extra intake of minerals is not needed. Excessive intake of Zinc may cause gastrointestinal problems and Pancytopenia (Irving 2003).
Matricaria recutita while Breastfeeding
SafeCAS Number: 520-36-5
It is a widely used plant even in infants. Because of lack of toxicity, a moderate use is considered to be safe. If topically used, do not apply it on the nipple because risk of contact dermatitis has been reported. There are two different species with similar properties: 1) Common or Sweet Chamomile (Matricaria recutita or Chamomilla recutita). 2) Roman, English or Bitter Chamomile (Anthemis nobilis o Chamaemelum nobile). Inflorescence of the herb is used. Contains Essential Oil, Flavonoids, Lactones and Tannins. Unproven properties are: Anti-spasmodic. Digestive, Anti-inflammatory, Sedative.
Echinacea, unspecified while Breastfeeding
Low RiskCAS Number: 84696-11-7
Plant that is widely used even during pregnancy and breastfeeding. Because a lack of toxicity with an appropriate dose and moderate consumption it should be compatible with breastfeeding. The roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids among others. Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications are: common cold, bronchitis, skin lesions.Roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids ... Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications according to Commission E of German Ministry of Health: common cold, bronchitis, skin lesions. Contrary to the European Scientific Cooperative on Phytotherapy (ESCOP), the European Medication Agency does not recommend usage in younger than 12 years (allergy risk). Avoid using for longer than 8 weeks (risk for leukopenia)
Shingles Breastfeeding Analsys - 2
Arsenic trioxide while Breastfeeding
CAS Number: 1327-53-3
Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy. It might be possible to breastfeed safely during intermittent therapy with an appropriate period of breastfeeding abstinence; the manufacturer recommends an abstinence period of 1 week after the last dose. Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk.[1] Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant.[2]
Sulfur while Breastfeeding
CAS Number: 7704-34-9
Sulfur 5% to 10% in a petrolatum base is safe for topical use in children, including infants under 2 months of age.[1] This makes it a useful alternative to organic insecticides for treating scabies in nursing mothers; however, the petrolatum base makes undesirable for use on the breast.
Matricaria recutita while Breastfeeding
CAS Number: 8002-66-2
Two different plant species with similar effects are known as chamomile: German chamomile (Matricaria recutita) and Roman chamomile (Chamaemelum nobile). Both contain similar ingredients, including sesquiterpenes (e.g., bisabolol, farnesene), sesquiterpenelactones (e.g., chamazulene, matricin), flavonoids (e.g., apigenin, luteolin), and volatile oils. Chamomile is used orally as a sedative and for gastrointestinal conditions; it is used topically for wound healing. Both herbal and homeopathic preparations have been used to treat mastitis and cracked, bleeding nipples.[1] Chamomile has been used as a galactogogue;[2][3] however, no scientifically valid clinical trials support this use. Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[4] Chamomile is "generally recognized as safe" (GRAS) for use in food by the U.S. Food and Drug Administration as a spice, seasoning, or flavoring agent. No data exist on the safety of chamomile in nursing mothers or infants, although rare sensitization may occur (see below).[5] It has been safely and effectively used alone and with other herbs in infants for the treatment of colic, diarrhea, and other conditions,[6][7][8][9] so the smaller amounts expected (but not demonstrated) in breastmilk are likely not to be harmful with usual maternal doses. Note Clostridium botulinum (botulism) spores have been found in some loose-leaf chamomile teas sold in health food stores. Topical chamomile is a known sensitizing agent, even with homeopathic products.[10] Two women developed contact dermatitis of the nipples and areolas after applying Kamillosan ointment for cracked nipples. The product was purchased in England and contained 10.5% Roman chamomile extracts and oil. Reactions were confirmed to be caused by Roman chamomile by patch testing in both women. Drinking chamomile tea can exacerbate topical skin rashes and has caused anaphylaxis in sensitized individuals.[11] Chamomile has possible cross-reactivity with other members of the aster family (e.g., echinacea, feverfew, and milk thistle).[5] Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Echinacea, unspecified while Breastfeeding
CAS Number: 84696-11-7; 90028-20
Echinacea species (Echinacea angustifolia, Echinacea purpurea, Echinacea pallida) contain high molecular weight polysaccharides (e.g., heteroxylan, arabinogalactan) and lower molecular weight compounds (e.g., alkylamides, caffeoyl conjugates such as cichoric acid and echinacosides), but no single chemical is known to be responsible for echinacea's biological activity. Some products have been standardized based on echinacoside, and others on cichoric acid. Echinacea has no specific uses during breastfeeding, but is commonly used orally to treat or prevent upper respiratory infections. It is also used topically to treat skin infections. Excretion of some of the purportedly active alkamides was found in breastmilk in one mother. No data exist on the safety and efficacy of echinacea in nursing mothers or infants. In general, echinacea is well tolerated with gastrointestinal upset, diarrhea and constipation, skin rash and rarely allergic reactions reported. It may also alter the metabolism of some dugs metabolized by the P450 enzyme system. Some sources indicate that echinacea is safe in recommended doses,[1] while others recommend avoiding it during breastfeeding because of the lack of published safety data. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Shingles Breastfeeding Analsys - 3
Toxicodendron pubescens leaf and Breastfeeding
SafePoison ivy rash is caused by contact with poison ivy, a plant that grows almost everywhere in the United States. The sap of the poison ivy plant, also known as Toxicodendron radicans, contains oil called urushiol. This is the irritant that causes an allergic reaction and rash.
You dont even have to come in direct contact with the plant to have a reaction. The oil can linger on your gardening equipment, golf clubs, or even your shoes. Brushing against the plant � or anything thats touched it � can result in skin irritation, pain, and itching.
Poison ivy is not contagious. It cannot spread from person to person. It can, however, be spread in a few other scenarios. For example, a pet that encounters poison ivy leaves can carry the urushiol oil in its fur. When you touch the animal, you may pick up the oil and develop a rash. Clothing fibers can also spread poison ivys oil. If you touch poison ivy with a pair of pants or shirt and do not wash it after contact is made, you could develop another rash if you touch the clothing. You can also spread the oil to another person, if they come into contact with clothes that have touched poison ivy. A poison ivy rash cannot spread across your body either. If you come into contact with poison ivy that is burning, you may inhale plant compounds. This can lead to irritation in the lungs, airways, and eyes.
Poison ivy rash doesnt pose a serious risk to a pregnant woman or a developing baby. Your baby can get the rash only from touching something with the oil on it. And the liquid in the blisters doesnt contain urushiol, so the rash cant be spread by scratching or popping them. If you notice a new patch of rash on your baby a few days after the first one appears, its not because the rash has spread. If you have poison ivy it should not affect the milk and health of breastfed baby.
Homeopathic preparations of Poison ivy are used to treat pain, rheumatoid arthritis, menstrual period problems, swelling, and itchy skin disorders. Due to extreme dilution of poison ivy in homeopathic medicines its mostly safe in breastfeeding.
Sulfur and Breastfeeding
SafeNote: Study and data for tropical use only
Warning: Tropical usage in breast area shall be avoided to prevent the Thuja passing orally in Infants.
Thuja occidentalis leafy twig and Breastfeeding
Low RiskThuja is one of the most common remedies used for warts. Topical Usage of Thuja for wart is likely safe while breastfeeding. We do not have sufficient safety usage data for Thuja oral consumption, However its likely unsafe to use thuja orally while breastfeeding.
Warning: Tropical usage in breast area shall be avoided to prevent the Thuja passing orally in Infants.What should I do if already breastfed my kid after using Shingles?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Shingles is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Shingles, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Shingles has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Shingles, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Shingles in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
