Lidocaine 23% / Tetracaine 7% Cream while Breastfeeding
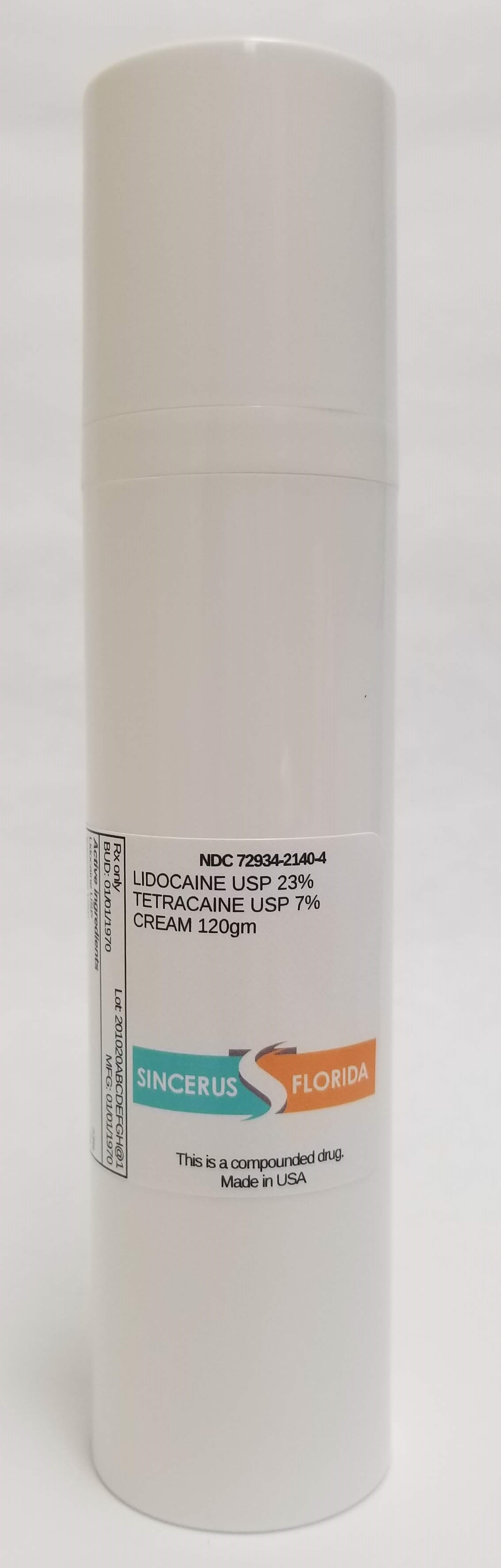
Lidocaine 23% / Tetracaine 7% Cream while breastfeeding safe or not? Can there be any side effects for infant while using it during breastfeeding?

Lidocaine 23% / Tetracaine 7% Cream Breastfeeding Analsys
Lidocaine while Breastfeeding
SafeCAS Number: 137-58-6
Compatible with breastfeeding no matter the multiple ways it can be used: anesthetic, anti-arrhythmic, or anti-epileptic drug. Excreted into breast milk in non-significant amount with no side effects on breastfed infants from treated mothers. As a topical anesthetic (dermatologic, dental-stomatologic, ophtalmotologic and otologic preparations) it has an almost nil systemic absorption. Avoid using it on the nipple, but if necessary do it after the breast feed, wipe it out and rinse with water before the next feed, An euptectic mixture with added Prilocaine (EMLA) is used for dermatologic anesthesia. There is an increased risk of Methemoglobinemia when applied on large surfaces or taken by mouth. Intrapartum anesthesia may delay the onset of phase II of Lactogenesis or milk coming-in. The American Academy of Pediatrics rates it usually compatible with Breastfeeding.
Tetracaine while Breastfeeding
SafeCAS Number: 94-24-6
Anesthetic drugs for topical use, both dermatological and odontological, have almost nil absorption when properly used. Do not apply on breast. Otherwise, do it after having nursed, and cleanse it thoroughly with water before next feeding.
Lidocaine 23% / Tetracaine 7% Cream Breastfeeding Analsys - 2
Lidocaine while Breastfeeding
CAS Number: 137-58-6
Lidocaine concentrations in milk during continuous IV infusion, epidural administration and in high doses as a local anesthetic are low and the lidocaine is poorly absorbed by the infant. Lidocaine is not expected to cause any adverse effects in breastfed infants. No special precautions are required.[1][2][3] Lidocaine labor and delivery with other anesthetics and analgesics has been reported by some to interfere with breastfeeding. However, this assessment is controversial and complex because of the many different combinations of drugs, dosages and patient populations studied as well as the variety of techniques used and deficient design of many of the studies. Overall it appears that with good breastfeeding support epidural lidocaine with or without fentanyl or one of its derivatives has little or no adverse effect on breastfeeding success.[4][5][6][7][8] Labor pain medication may delay the onset of lactation.
Tetracaine while Breastfeeding
CAS Number: 94-24-6
No information is available on the use of tetracaine during breastfeeding. Based on the low excretion of other local anesthetics into breastmilk, a single dose of injected tetracaine during breastfeeding, such as for a dental procedure, is unlikely to adversely affect the breastfed infant. However, an alternate drug may be preferred, especially while nursing a newborn or preterm infant. Topical application of tetracaine to the mother is unlikely to affect her breastfed infant if it is applied away from the breast. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[1]
What should I do if I am breastfeeding mother and I am already exposed to Lidocaine 23% / Tetracaine 7% Cream?
Lidocaine 23% / Tetracaine 7% Cream is safe in breastfeeding and should not create any health problem for your baby but in case you feel any health issue associated with Lidocaine 23% / Tetracaine 7% Cream you should contact your doctor or health care provider. Be it pregnancy or lactation you shall keep your doctor informed.
I am nursing mother and my doctor has suggested me to use Lidocaine 23% / Tetracaine 7% Cream, is it safe?
Definitely, Lidocaine 23% / Tetracaine 7% Cream is safe in lactation for baby. No wonder your doctor has recommended it.
If I am using Lidocaine 23% / Tetracaine 7% Cream, will my baby need extra monitoring?
No extra baby monitoring required while mother is using Lidocaine 23% / Tetracaine 7% Cream
Who can I talk to if I have questions about usage of Lidocaine 23% / Tetracaine 7% Cream in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
