Betamethasone Clotrimazole Cream while Breastfeeding
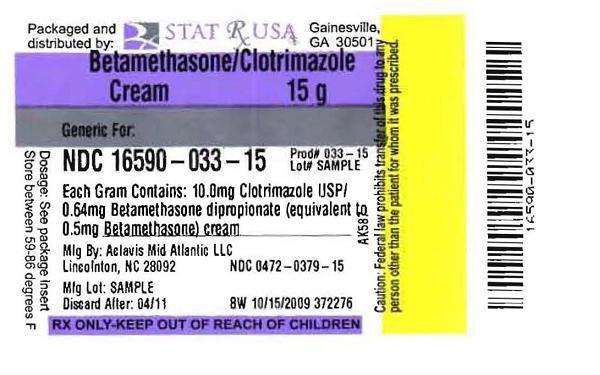
What is Betamethasone Clotrimazole Cream used for?
Betamethasone Clotrimazole Cream while breastfeeding safe or not? Can there be any side effects for infant while using it during breastfeeding?

Betamethasone Clotrimazole Cream Breastfeeding Analsys
Clotrimazole while Breastfeeding
SafeCAS Number: 23593-75-1
Excretion into breast milk is very unlikely since absorption through skin, vaginal mucosa, and, even intestinal mucosa into plasma is very poor with non-significant plasma levels or below the detection threshold (<10 ng/mL). In addition, because of a high plasma protein binding capacity, excretion into breast milk seems to be less likely. It is used frequently for treatment of Candida infection, either in skin or mouth mucosa, even in newborn and premature infants without observed side-effects. In case of use on the nipple, do it after feeding the baby and cleanse thoroughly the surface before the next one. Do not use creams, gels and other locally applied products that contain paraffin (mineral oil) to prevent absorption by the infant.
Betamethasone dipropionate while Breastfeeding
Low RiskCAS Number: 378-44-9
Because pharmacokinetic data suggest excretion into breast milk in significant levels long lasting treatments should use other steroidal drugs known to be excreted in low amounts. When administered before delivery it may induce delay in phase II of Lactogenesis (coming-in) and a decrease of milk production within the first week post-partum. Large intra-articular doses may transitory decrease milk production. WHO Model List of Essential Drugs 2002: Compatible with breastfeeding.
Betamethasone Clotrimazole Cream Breastfeeding Analsys - 2
Clotrimazole while Breastfeeding
CAS Number: 23593-75-1
Because clotrimazole has poor oral bioavailability, it is unlikely to adversely affect the breastfed infant, including topical application to the nipples. It has been used orally in infants with thrush, sometimes successfully after nystatin has failed.[1] Any excess cream or ointment should be removed from the nipples before nursing. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[2]
Betamethasone dipropionate while Breastfeeding
CAS Number: 378-44-9
Betamethasone ointment appears to have no advantage over lanolin for treating sore nipples during breastfeeding.[1] Since only extensive application of the most potent corticosteroids may cause systemic effects in the mother, it is unlikely that short-term application of topical corticosteroids would pose a risk to the breastfed infant by passage into breastmilk. However, it would be prudent to use the least potent drug on the smallest area of skin possible. It is particularly important to ensure that the infant's skin does not come into direct contact with the areas of skin that have been treated. Only the lower potency corticosteroids should be used on the nipple or areola where the infant could directly ingest the drugs from the skin; topical betamethasone should be avoided on the nipple.[2] Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[3] Any topical corticosteroid should be wiped off thoroughly prior to nursing if it is being applied to the breast or nipple area.
What if I already have used Betamethasone Clotrimazole Cream?
During whole lactation period you shall first discuss with your doctor and then together you shall decide whether you shall take that drug or not however if you have already taken Betamethasone Clotrimazole Cream then you shall inform your doctor, But you should not be worried too much as Betamethasone Clotrimazole Cream comes in category of low risk drug.
I am nursing mother and my doctor has suggested me to use Betamethasone Clotrimazole Cream, is it safe?
Betamethasone Clotrimazole Cream comes in category of low risk and if your doctor is aware that you are breastfeeding it should be ok to use
If I am using Betamethasone Clotrimazole Cream, will my baby need extra monitoring?
Not much
Who can I talk to if I have questions about usage of Betamethasone Clotrimazole Cream in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
