Vitality while Breastfeeding
What is Vitality used for?
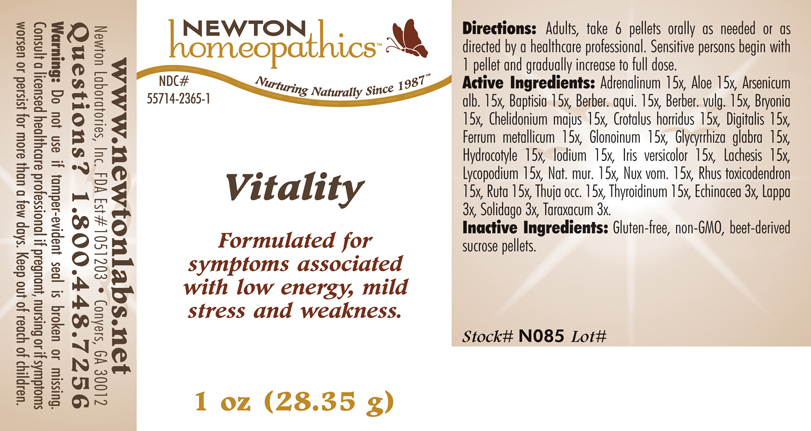
Brief: OTC - PURPOSE SECTION Formulated for symptoms associated with low energy, mild stress and weakness.
Is Vitality usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Vitality Breastfeeding Analsys
Epinephrine while Breastfeeding
SafeCAS Number: 51-43-4
Used as a systemic drug for cardiac resuscitation and locally in topical anesthetic preparations, epidural anesthesia, eye drops (mydriatic), and nasal drops (vasoconstrictor). At last update no published data on excretion in breast milk were found.Its rapid metabolism (short Tmax and T½) makes it unlikely an excretion into milk in significant amounts. It is destroyed in the gastrointestinal tract. The low oral-bioavailability makes its levels into infant's plasma, that would be absorbed from ingested breast milk, be nil or negligible. Maintained high intravenous doses decrease milk production by interfering with the secretion of prolactin especially the early postpartum-weeks, because when breastfeeding is well established, prolactin levels do not correlate with milk production any longer. No problems related to lactation have been observed due to epidural anesthesia in which adrenaline is used.
Aloe while Breastfeeding
Low RiskCAS Number: 8001-97-6
Herb leaves are used. It contains hydroxianthracenes, acemannan and glycomannan. Attributed properties: laxative and healing effect on wounds. Indication according to Commission E of the German Ministry of Health: constipation. Excessive or long-term use may lead to severe diarrhea, dehydration and liver toxicity. At latest update, relevant published data on excretion into breast milk were not found.As an active laxative compound it can lead to colicky abdominal pain. Because excretion into breast milk is possible, avoiding it while breastfeeding is advisable. Non-toxic when topically used. Without proof of efficacy it is used to treat nipple's crackles or pain. If applied on the breast, cleanse it thoroughly before nursing to avoid swallowing by the infant. Risk of diarrhea or refusing to latch-on because of bad taste would increase.
Arsenic trioxide while Breastfeeding
DangerousUsed in the treatment of promyelocitic leukemia in adults.
Mahonia aquifolium root bark while Breastfeeding
Low RiskRoots and bark of plant are used. It is popularly used as a topical medication for several skin affections like psoriasis, acne and fungal infections. Controlled studies have failed to show any effectiveness or that is similar to placebo. It contains Berberine that may be a cause of gastritis, nephritis, phototoxicity and severe jaundice by displacement of albumin-linked bilirubin: it places a risk of kernicterus to newborns, which is greater in cases of 6-Glucose-PD deficiency.
Berberis vulgaris root bark while Breastfeeding
DangerousCAS Number: 84649-92-3
Roots and bark are used. It contains Berberine that may be a cause of gastritis, nephritis, phototoxicity and severe jaundice by displacement of albumin -linked bilirubin: higher risk of kernicterus to newborns, which is greater in cases of 6-Glucose-PD deficiency. It is popularly widely used, however, its effectiveness has not been shown. Use not approved by the Commission E of German Ministry of Health. It should be avoided.
Bryonia alba root while Breastfeeding
Low RiskClimbing plant. The female inflorescences or flower tips are used.It contains phloroglucinols, estrogenic, quercetin, kaempferol, tannins, phenolic acids essential oil and flavonoids. One of its components, 8-prenylnaringenin (8-PN) is the most powerful phytoestrogen known. Properties that are attributed: hypnotic, sedative, orexigenic.It is used as a flavoring and stabilizer of the beer.Indications German Commission E Ministry of Health, EMA and ESCOP: insomnia, nervousness, anxiety There is no scientific evidence showing an improvement in milk production.A possible estrogenic effect may be a decrease in milk production.The best galactogogue is a frequent and on-demand breastfeeding along with proper technique. During breastfeeding its consumption should be moderate or occasional.
Iron while Breastfeeding
SafeSeveral ferrous salts of iron (ascorbate, aspartate, citrate, chloride, fumarate, gluconate, lactate, oxalate, succinate, sulfate, glycine sulfate, etc.) are used in oral administration for treating or preventing iron deficiency anemia.Its molecular weight varies from 170 for the fumarate and succinate, and from 280 for lactate and sulfate to 400 for aspartate and ascorbate. Characteristics of iron metabolism in the body make unlikely that it would be excreted in a significant amount into breast milk.It is a medication used for treatment of Neonatal Anemia in premature babies. Iron is excreted in small amounts in human milk, usually being enough for covering the daily needs of infants due to its high bioavailability. There is no correlation between mother's daily intake of iron and its concentration in breast milk.Iron supplementation to the mother does not increase levels of iron in breast milk or infant plasma significantly. Excessive supplementation can reduce the zinc concentration in milk. WHO List of Essential Medicines 2002: compatible with breastfeeding.
Nitroglycerin while Breastfeeding
SafeCAS Number: 55-63-0
Vasodilator used to treat cardiac disorders like ischemia and mainly anal fissures.It is also used during pregnancy as a tocolytic drug in cases of threatened preterm labor and eclampsia.It has been used to treat heart disorders in babies and children. Even to treat anal fissures in children under 1 year, and noteworthy, in ischemic issues on premature infants without side effects.It is administered intravenously, orally, sublingually, on skin patches, ointment ... Because of a moderately-high volume of distribution and very fast metabolism (Tmax and t1 / 2 minutes) it is highly unlikely the passage of significant amounts to the breast milk, especially when applied topically. This explains why it has not been observed any troubles in 40 infants whose mothers with anal fissures were treated with nitroglycerin ointment application even for periods of 12 months. Mothers have complained of headaches that commonly occur with the use of various vasodilators drugs. The amount of nitrate / nitrite in this type of vasodilator drugs is of few milligrams, therefore, toxicity associated to nitrates such as methemoglobinemia in breastfed infants from treated mothers has not been reported (The dose of nitrite is Rectogesic 1.5 mg / 12 hours).
Glycyrrhiza glabra while Breastfeeding
UnsafeCAS Number: 1405-86-3
Root of leguminous herb is used. Content: essential oil, flavonoids, tannins, saponins, hydroxi-coumarins.... Unproven effects: anti-ulcerative and expectorant. Indication after Commission E of German Ministry of Health: gastritis, gastric ulcer, cough, bronchitis. Because of mineralocorticoid effects, Pseudoaldosteronism, Hypokalemic palsy, Hypernatremia, Edema, Heart arrhythmias and Arterial Hypertension, a longstanding use or abuse of licorice may be a cause of severe health disorders. May be a cause of abortion and premature labor if taken while pregnancy. Since it has anti-prolactin and estrogenic effects, decrease of milk production can occur within the first weeks after birth. Reportedly, one case of hyperprolactinemia has occurred. There is no proof on its galactagogue effect. Glycyrrhizin is responsible of many effects of Licorice which is excreted in small amount into breast milk. Two infants younger than one months were severely intoxicated (lethargy) after their mothers had drunk an daily average of 2 liters of a beverage containing a mixture of Licorice, Fennel, Anise and Goat's rue. It was assumed to be related to anethol contained in the fennel and anise.
Centella asiatica while Breastfeeding
SafeAt latest update, relevant published data on excretion into breast milk were not found. It contains triterpenic saponins (asiaticoside and madecassoside), tannins, phytosterols and essential oil. Frequent and exaggerated use of triterpenes may cause liver damage. Properties that are attributed for topical use (some clinically tested) like are healing of wound and venous tonic. There is no proof on effectiveness when used by mouth. Because of a low or nil systemic absorption through skin or vaginal mucosa, the topical use is believed be compatible with breastfeeding. Do not use it on the breast or clean it thoroughly to avoid ingestion by the infant. Avoid oral administration.
Iodine while Breastfeeding
UnsafeCAS Number: 7553-56-2
Disinfectant that contains high amount (2-7%) of Iodine in solution with alcohol or water (Lugol's solution) Not absorbed through intact skin of adults. However, it may trespass the inflamed skin, wounds, mucosa surfaces like vagina, in which case can reach concentration in grams in the human serum (1 g = 1,000 milligrams = 1,000,000 micrograms). Normal daily allowance is considered to be as high as 100 to 150 micrograms that increases to 200 – 300 micrograms in pregnancy or nursing period. The latter means less than one third of a milligram. Iodine is concentrated into breast milk with a level that could reach 20 times higher than the concentration in the blood. It has been found higher levels of Iodine, altered results of neonatal screening test for thyroid function, and, transient hypothyroidism in infants whose mothers were exposed to Iodine Povidone. Use should be avoid in the Delivery Room, Operating Room (C-section), Neonatal Units, Toddler admision areas and during the breastfeeding period. Sporadic or inadvertent use, specially on normal skin, does not require special test or procedures because it does not pose higher risk to the child.
Lycopodium clavatum spore while Breastfeeding
UnsafeAerial summits and spores of this fern are used. Traditionally use as a diuretic and intestinal spasm relief drug. Also used for abrasions and skin irritation. It may be a cause of asthma and contact dermatitis.
Sodium chloride while Breastfeeding
SafeCAS Number: 7647-14-5
Sodium chloride either as cooking salt, or, as oral rehydration solution, or, as IV fluid, is entirely compatible with BF.
Strychnos nux-vomica seed while Breastfeeding
DangerousCAS Number: 8046-97-7
Dried seed of this plant has been used. It contains brucine and strychnine. It is highly toxic and easily lethal.
Echinacea, unspecified while Breastfeeding
Low RiskCAS Number: 84696-11-7
Plant that is widely used even during pregnancy and breastfeeding. Because a lack of toxicity with an appropriate dose and moderate consumption it should be compatible with breastfeeding. The roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids among others. Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications are: common cold, bronchitis, skin lesions.Roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids ... Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications according to Commission E of German Ministry of Health: common cold, bronchitis, skin lesions. Contrary to the European Scientific Cooperative on Phytotherapy (ESCOP), the European Medication Agency does not recommend usage in younger than 12 years (allergy risk). Avoid using for longer than 8 weeks (risk for leukopenia)
Arctium lappa root while Breastfeeding
Low RiskThe root is used. It contains inulin, mucilage, phenol acids and phytosterols. Indication after Commission E of German Ministry of Health: none, since no beneficial effect has been shown.
Solidago virgaurea flowering top while Breastfeeding
SafeCAS Number: 85117-06-2
Perennial plant. Florid summits are used.It contains flavonoids, tannins, saponosides.Indication after Commission E of German Ministry of Health: diuretic. Daily dose: 6 to 12 g of drug or equivalent. Be cautious with extracted alcohol and tincture.
Taraxacum officinale while Breastfeeding
SafeThe roots and leaves of the plant in salads both as food and herbal medicine are used.It contains inulin, terpenes, phytosterols, flavonoids, coumarins and potassium salts in large quantities.Attributed Properties: cholagogue, laxative, orexigenic. diureticIndication by the German Commission E Ministry of Health: dyspepsia, cholelithiasis, anorexia.Indications by the European Medicament Agency (EMA): diuretic. Non toxic. There is no evidence of its effectiveness as galactogogue.Best galactogogue is a frequent on-demand breastfeeding and proper technique. Its wide use, low toxicity and since it is also consumed as food, a moderate consumption during lactation is considered of little or no risk. Precaution is recommended before taking herbal infusions:1. Ensure a reliable source: poisoning occurred by confusion with another plant that resulted to be toxic, poisoning from heavy metals and food poisoning by contamination with bacteria or fungi.2. Avoid excessive consumption. The "natural" products are not good in any amount: plants contain active substances from which come out much of our traditional pharmacopoeia and can cause poisoning if eaten in exaggerated quantity or prolonged time.
Vitality Breastfeeding Analsys - 2
Epinephrine while Breastfeeding
CAS Number: 51-43-4
No information is available on the use of epinephrine during breastfeeding. Because of its poor oral bioavailability and short half-life, any epinephrine in milk is unlikely to affect the infant. High intravenous doses of epinephrine might reduce milk production or milk letdown. Low-dose intramuscular (such as Epi-Pen), epidural, topical, inhaled or ophthalmic epinephrine are unlikely to interfere with breastfeeding. To substantially diminish the effect of the drug after using eye drops, place pressure over the tear duct by the corner of the eye for 1 minute or more, then remove the excess solution with an absorbent tissue.
Aloe while Breastfeeding
CAS Number: 8001-97-6
Aloe vera gel consists of the clear gel from the center of fresh leaves of Aloe vera and related aloes. Active ingredients include mono- and polysaccharides (e.g., acemannan, glucomannan), allantoin, enzymes (e.g., cyclooxygenase, amylase, lipase, alkaline phosphatase, carboxypeptidase), and salicylic acid. It should not be confused with Aloe latex which comes from the inner portion of the skin and contains potent anthraquinone laxatives. Aloe vera gel has been used topically on the nipples during nursing to help heal cracked nipples. In a randomized, single-blinded study (investigators blinded), aloe vera was more effective than lanolin in decreasing nipple pain score after 7 days in women with sore nipples postpartum.[1] Another study compared breastmilk alone applied to the nipples after breastfeeding to either olive oil or aloe vera gel. All had less pain after 7 days of nursing, but the decrease on pain was greater with aloe vera than with the other treatments.[2] Topical aloe has also been combined with a cactus leaf preparation and massage to treat engorgement.[3] If aloe vera is applied to the nipples, it should be washed off before nursing the infant because the taste might adversely affect nursing or cause diarrhea in the infant.[4][5] No data exist on the safety and efficacy of Aloe vera gel in nursing mothers or infants. Aloe vera gel has caused itching, burning, and allergic contact dermatitis, possibly from contamination with the irritating latex from the leaves.[6][7] Aloe vera gel also has an antiplatelet effect and can enhance the antiplatelet effect of other drugs. Aloe latex, the laxative, should not be used during breastfeeding.[8][9] Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Arsenic trioxide while Breastfeeding
CAS Number: 1327-53-3
Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy. It might be possible to breastfeed safely during intermittent therapy with an appropriate period of breastfeeding abstinence; the manufacturer recommends an abstinence period of 1 week after the last dose. Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk.[1] Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant.[2]
Nitroglycerin while Breastfeeding
CAS Number: 55-63-0
Topical use of nitroglycerin for anal fissures by nursing mothers appears to have no adverse effects on their breastfed infants. Topical use on the nipples has been used for alleviation of Raynaud phenomenon of the nipples, but only after cessation of breastfeeding.[1] Nitroglycerin should not be used topically on the nipples during breastfeeding. Sublingual and intravenous nitroglycerin have not been studied during breastfeeding. Observe infants for flushing and discomfort after breastfeeding.
Glycyrrhiza glabra while Breastfeeding
CAS Number: 84775-66-6
Licorice (Glycyrrhiza glabra) root contains glycyrrhizin (also called glycyrrhizic acid or glycyrrhizinic acid) and a mixture of the potassium and calcium salts of glycyrrhizic acid. Glycyrrhizin is metabolized to the active glycyrrhetinic acid in the intestine. Deglycyrrhizinated licorice (DGL) has had glycyrrhizin removed. Licorice is a purported galactogogue, and is included in some Asian proprietary mixtures to increase milk supply; however, no scientifically valid clinical trials support this use. In fact, licorice usually reduces serum prolactin,[1] which might decrease milk production in the early stages of lactation. Women taking licorice have experienced elevated blood presure.[2] Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[3] Glycyrrhizin is detectable in the breastmilk of some women taking licorice, but studies measuring glycyrrhetinic acid have not been performed. Licorice has been used safely and effectively in combination with other herbs given to infants as a tea for the short-term treatment of colic.[4] However, two infants whose mothers had an excessive intake of an herbal tea that contained licorice had signs of anethole toxicity.[5] Because both of these papers reported on herbal mixtures, the effect(s) of licorice alone cannot be determined. Licorice and licorice extract are "generally recognized as safe" (GRAS) as foods by the U.S. Food and Drug Administration. Long-term, excessive use of licorice can cause hypertension, hypokalemia, and disturbances of adrenal hormones, and therefore should probably be avoided during nursing. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Iodine while Breastfeeding
CAS Number: 7553-56-2
Iodine is an essential trace nutrient for all infants that a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in fullterm infants and 30 mcg/kg daily in premature infants.[1] Systematic reviews and studies on iodine nutrition found that iodine in breastmilk is adequate in iodine-sufficient countries, but in countries with iodine fortification of foods, many mothers did not obtain adequate iodine and that additional supplementation was desirable.[2][3][4][5] In iodine-deficient areas, supplementation of breastfeeding mothers with iodine appears to be more effective than direct supplementation of the infant in reducing infant iodine deficiency.[6] The American Thyroid Association recommends that breastfeeding women should supplement their diet with a daily oral supplement that contains 150 mcg of iodine, but sustained iodine intake while breastfeeding that exceeds 500 to 1100 mcg daily should be avoided.[7] A survey in the United States between 2011 and 2014 found that only 19% of lactating women used a dietary supplement that contained iodine.[8] The use of excessive amounts of iodine in the mother near term and during breastfeeding (e.g., seaweed soup) can increase breastmilk iodine levels and cause transient hypothyroidism in breastfed infants. The absorption of iodine can be marked after application to open wounds or mucous membranes. Exposure of mothers to unnecessary iodine who are or will be breastfeeding should be avoided or minimized to the extent possible by avoiding its use on maternal mucous membranes (e.g., vaginal use, wound therapy), avoiding prolonged contact time, avoiding repeated applications, and applying it to the smallest possible surface areas of the body. It is possible that maternal exposure to iodine near term could interfere with thyroid studies done as a part of newborn screening tests.
Thyroid, unspecified while Breastfeeding
CAS Number: 8028-36-2
Thyroid is an animal-derived mixture of levothyroxine (T4) and liothyronine (T3), which are normal components of human milk. Limited data on exogenous replacement doses of levothyroxine during breastfeeding indicate no adverse effects in infants. If thyroid is required by the mother, it is not a reason to discontinue breastfeeding. The American Thyroid Association recommends that subclinical and overt hypothyroidism should be treated with levothyroxine in lactating women seeking to breastfeed.[1] Thyroid dosage requirement may be increased in the postpartum period compared to prepregnancy requirements patients with Hashimoto's thyroiditis.[2]
Echinacea, unspecified while Breastfeeding
CAS Number: 84696-11-7; 90028-20
Echinacea species (Echinacea angustifolia, Echinacea purpurea, Echinacea pallida) contain high molecular weight polysaccharides (e.g., heteroxylan, arabinogalactan) and lower molecular weight compounds (e.g., alkylamides, caffeoyl conjugates such as cichoric acid and echinacosides), but no single chemical is known to be responsible for echinacea's biological activity. Some products have been standardized based on echinacoside, and others on cichoric acid. Echinacea has no specific uses during breastfeeding, but is commonly used orally to treat or prevent upper respiratory infections. It is also used topically to treat skin infections. Excretion of some of the purportedly active alkamides was found in breastmilk in one mother. No data exist on the safety and efficacy of echinacea in nursing mothers or infants. In general, echinacea is well tolerated with gastrointestinal upset, diarrhea and constipation, skin rash and rarely allergic reactions reported. It may also alter the metabolism of some dugs metabolized by the P450 enzyme system. Some sources indicate that echinacea is safe in recommended doses,[1] while others recommend avoiding it during breastfeeding because of the lack of published safety data. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Vitality Breastfeeding Analsys - 3
Baptisia tinctoria and Breastfeeding
UnsafeWild indigo is an herb. The root is used to make medicine.Wild indigo is used for infections such as diphtheria, influenza (flu), swine flu, the common cold and other upper respiratory tract infections, lymph node infections, scarlet fever, malaria, and typhoid. It is also used for sore tonsils (tonsillitis), sore throat, swelling of the mouth and throat, fever, boils, and Crohns disease. Some people apply wild indigo directly to the skin for ulcers, sore and painful nipples, as a douche for vaginal discharge, and for cleaning open and swollen wounds. Wild indigo is UNSAFE when taken by mouth or applied to the skin, long-term or in large doses. Large doses can cause vomiting, diarrhea, other intestinal problems, and spasms.
While breastfeeding wild indigo is likely not safe when taken by mouth or applied to the skin. Avoid use.
Toxicodendron pubescens leaf and Breastfeeding
SafePoison ivy rash is caused by contact with poison ivy, a plant that grows almost everywhere in the United States. The sap of the poison ivy plant, also known as Toxicodendron radicans, contains oil called urushiol. This is the irritant that causes an allergic reaction and rash.
You dont even have to come in direct contact with the plant to have a reaction. The oil can linger on your gardening equipment, golf clubs, or even your shoes. Brushing against the plant � or anything thats touched it � can result in skin irritation, pain, and itching.
Poison ivy is not contagious. It cannot spread from person to person. It can, however, be spread in a few other scenarios. For example, a pet that encounters poison ivy leaves can carry the urushiol oil in its fur. When you touch the animal, you may pick up the oil and develop a rash. Clothing fibers can also spread poison ivys oil. If you touch poison ivy with a pair of pants or shirt and do not wash it after contact is made, you could develop another rash if you touch the clothing. You can also spread the oil to another person, if they come into contact with clothes that have touched poison ivy. A poison ivy rash cannot spread across your body either. If you come into contact with poison ivy that is burning, you may inhale plant compounds. This can lead to irritation in the lungs, airways, and eyes.
Poison ivy rash doesnt pose a serious risk to a pregnant woman or a developing baby. Your baby can get the rash only from touching something with the oil on it. And the liquid in the blisters doesnt contain urushiol, so the rash cant be spread by scratching or popping them. If you notice a new patch of rash on your baby a few days after the first one appears, its not because the rash has spread. If you have poison ivy it should not affect the milk and health of breastfed baby.
Homeopathic preparations of Poison ivy are used to treat pain, rheumatoid arthritis, menstrual period problems, swelling, and itchy skin disorders. Due to extreme dilution of poison ivy in homeopathic medicines its mostly safe in breastfeeding.
Thuja occidentalis leafy twig and Breastfeeding
Low RiskThuja is one of the most common remedies used for warts. Topical Usage of Thuja for wart is likely safe while breastfeeding. We do not have sufficient safety usage data for Thuja oral consumption, However its likely unsafe to use thuja orally while breastfeeding.
Warning: Tropical usage in breast area shall be avoided to prevent the Thuja passing orally in Infants.Thyroid, unspecified and Breastfeeding
SafeI already used Vitality and meanwhile I breastfed my baby should I be concerned?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Vitality is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Vitality, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Vitality has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Vitality, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Vitality in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
