Metronidazole Cream while Breastfeeding
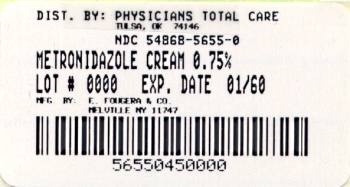
What is Metronidazole Cream used for?
Is Metronidazole Cream usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Nursing mothers: After oral administration, metronidazole is secreted in breast milk in concentrations similar to those found in the plasma. Even though blood levels are significantly lower with topically applied metronidazole than those achieved after oral administration of metronidazole, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Metronidazole Cream Breastfeeding Analsys
Metronidazole while Breastfeeding
SafeCAS Number: 443-48-1
Excreted into breast milk in a non-significant clinical amount. Not problems on breastfed infants of treated mothers were found. Plasma levels were low or undetectable in those infants. For a mother's dose of 400 mg three times-a-day, the intake of a breastfed infant would be less than 10% of the usual daily pediatric dose, whenever the breast-feed is done within 2-3 hours of mother's intake. Widely used for treatment of Giardia lamblia infections, even in small infants, without adverse effects reported. Metronidazole may produce a red discoloration of corporal fluids and bitter flavor of the milk with no harm effect on the child.
Metronidazole Cream Breastfeeding Analsys - 2
Metronidazole while Breastfeeding
CAS Number: 443-48-1
With maternal intravenous and oral therapy, breastfed infants receive metronidazole in doses that are less than those used to treat infections in infants, although the active metabolite adds to the total infant exposure. Plasma levels of the drug and metabolite are measurable, but less than maternal plasma levels. Case reports of candidal infections and diarrhea have been reported, and a comparative trial suggested that oral and rectal colonization with might be more common in infants exposed to metronidazole. Neither topical nor vaginal metronidazole have been studied during breastfeeding. After vaginal administration, plasma levels are less than 2% of those after a 500 mg oral dose. After topical administration, blood levels are about 1% of the peak plasma levels after a 250 mg oral dose. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[1] Because of the well demonstrated genotoxicity and mutagenicity in bacteria, carcinogenicity in animals, and possible mutagenicity in humans,[2][3] concern has been raised about exposure of healthy infants to metronidazole via breastmilk.[4] The relevance of these findings has been questioned and no definitive study has yet been performed in humans.[3][5] Opinions vary among experts on the advisability of using metronidazole during longer-term therapy while breastfeeding, but some sources recommend discontinuing breastfeeding for 12 to 24 hours after single-dose maternal treatment.[4][6] Other drugs are available for some conditions that metronidazole is used to treat. Topical or vaginal use of metronidazole during breastfeeding is unlikely to be of concern, although the manufacturer of one vaginal product recommends not breastfeeding during treatment and for 2 days after the last dose.
I am nursing mother and I have already used Metronidazole Cream, what should I do?
As usage of Metronidazole Cream is mostly safe while breastfeeding hence there should not be any concern. In case of any change in behavior or health of your baby you should inform your health care provider about usage of Metronidazole Cream else no further action is required.
I am nursing mother and my doctor has suggested me to use Metronidazole Cream, is it safe?
Definitely, Metronidazole Cream is safe in lactation for baby. No wonder your doctor has recommended it.
If I am using Metronidazole Cream, will my baby need extra monitoring?
No extra baby monitoring required while mother is using Metronidazole Cream
Who can I talk to if I have questions about usage of Metronidazole Cream in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
