There are high number of clear evidence that breastfeeding provides best nutrition that you can give to your baby. It is also evident that lactation is good for mothers health as well. Evolution has designed breastfeeding in a way that it caters all nutritional need of your child. However modern medicine is quite new for evolution, that is why mothers body is not well prepared to filter unnecessary chemical found in medicines. It becomes a necessity to figure out which drug is safe and which drug is dangerous for your newborn while nursing. In this article we will understand function of Levaquin | Levofloxacin Tablet and its suitability with breastfeeding.
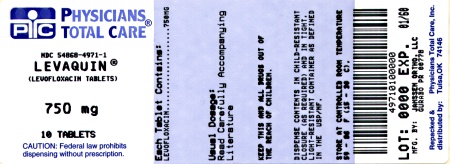
What is Levaquin | Levofloxacin Tablet used for?
To reduce the development of drug-resistant bacteria and maintain the effectiveness of LEVAQUIN® and other antibacterial drugs, LEVAQUIN® should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy. LEVAQUIN® Tablets/Injection and Oral Solution are indicated for the treatment of adults (≥18 years of age) with mild, moderate, and severe infections caused by susceptible strains of the designated microorganisms in the conditions listed in this section. LEVAQUIN® Injection is indicated when intravenous administration offers a route of administration advantageous to the patient (e.g., patient cannot tolerate an oral dosage form). LEVAQUIN® is a fluoroquinolone antibacterial indicated in adults (≥18 years of age) with infections caused by designated, susceptible bacteria (1, 12.4). Pneumonia: nosocomial (1.1) and community acquired (1.2, 1.3) Acute bacterial sinusitis (1.4) Acute bacterial exacerbation of chronic bronchitis (1.5) Skin and skin structure infections: complicated (1.6) and uncomplicated (1.7) Chronic bacterial prostatitis (1.8) Urinary tract infections: complicated (1.9, 1.10) and uncomplicated (1.12) Acute pyelonephritis (1.11) Inhalational anthrax, post-exposure (1.13). Not tested in humans for post-exposure prevention of inhalational anthrax; plasma concentrations are likely to predict efficacy (14.9) Culture and susceptibility testing Appropriate culture and susceptibility tests should be performed before treatment in order to isolate and identify organisms causing the infection and to determine their susceptibility to levofloxacin [see Clinical Pharmacology (12.4)]. Therapy with LEVAQUIN® may be initiated before results of these tests are known; once results become available, appropriate therapy should be selected. As with other drugs in this class, some strains of Pseudomonas aeruginosa may develop resistance fairly rapidly during treatment with LEVAQUIN®. Culture and susceptibility testing performed periodically during therapy will provide information about the continued susceptibility of the pathogens to the antimicrobial agent and also the possible emergence of bacterial resistance. 1.1 Nosocomial Pneumonia LEVAQUIN® is indicated for the treatment of nosocomial pneumonia due to methicillin-susceptible Staphylococcus aureus, Pseudomonas aeruginosa, Serratia marcescens, Escherichia coli, Klebsiella pneumoniae, Haemophilus influenzae, or Streptococcus pneumoniae. Adjunctive therapy should be used as clinically indicated. Where Pseudomonas aeruginosa is a documented or presumptive pathogen, combination therapy with an anti-pseudomonal β-lactam is recommended [see Clinical Studies (14.1)]. 1.2 Community-Acquired Pneumonia: 7–14 day Treatment Regimen LEVAQUIN® is indicated for the treatment of community-acquired pneumonia due to methicillin-susceptible Staphylococcus aureus, Streptococcus pneumoniae (including multi-drug-resistant Streptococcus pneumoniae [MDRSP]), Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Moraxella catarrhalis, Chlamydophila pneumoniae, Legionella pneumophila, or Mycoplasma pneumoniae [see Dosage and Administration (2.1) and Clinical Studies (14.2)]. MDRSP isolates are strains resistant to two or more of the following antibacterials: penicillin (MIC ≥2 mcg/mL), 2nd generation cephalosporins, e.g., cefuroxime, macrolides, tetracyclines and trimethoprim/sulfamethoxazole. 1.3 Community-Acquired Pneumonia: 5-day Treatment Regimen LEVAQUIN® is indicated for the treatment of community-acquired pneumonia due to Streptococcus pneumoniae (excluding multi-drug-resistant strains [MDRSP]), Haemophilus influenzae, Haemophilus parainfluenzae, Mycoplasma pneumoniae, or Chlamydophila pneumoniae [see Dosage and Administration (2.1) and Clinical Studies (14.3)]. 1.4 Acute Bacterial Sinusitis: 5-day and 10–14 day Treatment Regimens LEVAQUIN® is indicated for the treatment of acute bacterial sinusitis due to Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis [see Clinical Studies (14.4)]. 1.5 Acute Bacterial Exacerbation of Chronic Bronchitis LEVAQUIN® is indicated for the treatment of acute bacterial exacerbation of chronic bronchitis due to methicillin-susceptible Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Haemophilus parainfluenzae, or Moraxella catarrhalis. 1.6 Complicated Skin and Skin Structure Infections LEVAQUIN® is indicated for the treatment of complicated skin and skin structure infections due to methicillin-susceptible Staphylococcus aureus, Enterococcus faecalis, Streptococcus pyogenes, or Proteus mirabilis [see Clinical Studies (14.5)]. 1.7 Uncomplicated Skin and Skin Structure Infections LEVAQUIN® is indicated for the treatment of uncomplicated skin and skin structure infections (mild to moderate) including abscesses, cellulitis, furuncles, impetigo, pyoderma, wound infections, due to methicillin-susceptible Staphylococcus aureus, or Streptococcus pyogenes. 1.8 Chronic Bacterial Prostatitis LEVAQUIN® is indicated for the treatment of chronic bacterial prostatitis due to Escherichia coli, Enterococcus faecalis, or methicillin-susceptible Staphylococcus epidermidis [see Clinical Studies (14.6)]. 1.9 Complicated Urinary Tract Infections: 5-day Treatment Regimen LEVAQUIN® is indicated for the treatment of complicated urinary tract infections due to Escherichia coli, Klebsiella pneumoniae, or Proteus mirabilis [see Clinical Studies (14.7)]. 1.10 Complicated Urinary Tract Infections: 10-day Treatment Regimen LEVAQUIN® is indicated for the treatment of complicated urinary tract infections (mild to moderate) due to Enterococcus faecalis, Enterobacter cloacae, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, or Pseudomonas aeruginosa [see Clinical Studies (14.8)]. 1.11 Acute Pyelonephritis: 5 or 10-day Treatment Regimen LEVAQUIN® is indicated for the treatment of acute pyelonephritis caused by Escherichia coli, including cases with concurrent bacteremia [see Clinical Studies (14.7, 14.8)]. 1.12 Uncomplicated Urinary Tract Infections LEVAQUIN® is indicated for the treatment of uncomplicated urinary tract infections (mild to moderate) due to Escherichia coli, Klebsiella pneumoniae, or Staphylococcus saprophyticus. 1.13 Inhalational Anthrax (Post-Exposure) LEVAQUIN® is indicated for inhalational anthrax (post-exposure) to reduce the incidence or progression of disease following exposure to aerosolized Bacillus anthracis. The effectiveness of LEVAQUIN® is based on plasma concentrations achieved in humans, a surrogate endpoint reasonably likely to predict clinical benefit. LEVAQUIN® has not been tested in humans for the post-exposure prevention of inhalation anthrax. The safety of LEVAQUIN® in adults for durations of therapy beyond 28 days or in pediatric patients for durations of therapy beyond 14 days has not been studied. Prolonged LEVAQUIN® therapy should only be used when the benefit outweighs the risk [see Dosage and Administration (2.1, 2.2) and Clinical Studies (14.9)].
I am breastfeeding mother and I am using Levaquin | Levofloxacin Tablet. Can it have any bad effect on my kid? Shall I search for better alternative?
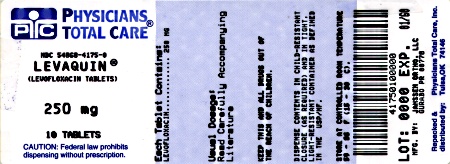
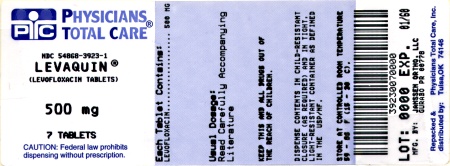
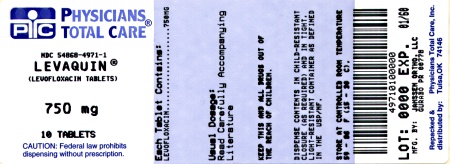
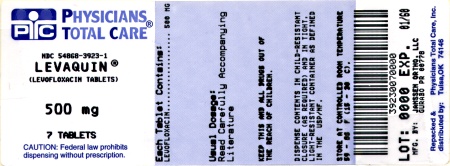
Levofloxacin is the one and only active ingredient present in Levaquin | Levofloxacin Tablet. Levofloxacin in itself is a low risk drug for lactation so it is easy to understand that Levaquin | Levofloxacin Tablet also comes in category of Low Risk item while breastfeeding. Below is the summary of Levofloxacin in breastfeeding.
Statement of Manufacturer/Labeler about breastfeeding usage
8.3 Nursing Mothers Based on data on other fluoroquinolones and very limited data on LEVAQUIN®, it can be presumed that levofloxacin will be excreted in human milk. Because of the potential for serious adverse reactions from LEVAQUIN® in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Levaquin | Levofloxacin Tablet Breastfeeding Analsys
Low RiskCAS Number: 100986-85-4
Is the S-isomer of ofloxacin. Recently, quinolone-related medication has been used in neonates and infants without apparent side effects. It trespasses in tiny amounts into breast milk. Absorption through the child’s gut may be interfered by the calcium contained in the milk. Should it be necessary to prescribe it to a nursing mother, Norfloxacine, Ofloxacine and Ciprofloxacine have shown a lower level in the milk and thus must be the preferred drugs. Because a case of pseudomembranose colitis has been described possibly related to mother ingestion of Ciporfloxacine in a premature infant previously affected of NEC, a close follow-up for diarrhea is warranted. Be aware of the possibility of false negative results of bacterial cultures when the mother is on antibiotics.
Levaquin | Levofloxacin Tablet Breastfeeding Analsys - 2
CAS Number: 100986-85-4
Levofloxacin is the -enantiomer of the fluoroquinolone, ofloxacin. No information is available on the clinical use of levofloxacin during breastfeeding. However, amounts in breastmilk appear to be low and would not be expected to cause any adverse effects in breastfed infants. Fluoroquinolones such as levofloxacin have traditionally not been used in infants because of concern about adverse effects on the infants' developing joints. However, recent studies indicate little risk.[1][2] The calcium in milk might prevent absorption of the small amounts of fluoroquinolones in milk,[3] but insufficient data exist to prove or disprove this assertion. Use of levofloxacin is acceptable in nursing mothers with monitoring of the infant for possible effects on the gastrointestinal flora, such as diarrhea or candidiasis (thrush, diaper rash). Avoiding breastfeeding for 4 to 6 hours after a dose should decrease the exposure of the infant to levofloxacin in breastmilk. Maternal use of an eye drop that contains levofloxacin presents negligible risk for the nursing infant.
What should I do if I am breastfeeding mother and I am already exposed to Levaquin | Levofloxacin Tablet?
During whole lactation period you shall first discuss with your doctor and then together you shall decide whether you shall take that drug or not however if you have already taken Levaquin | Levofloxacin Tablet then you shall inform your doctor, But you should not be worried too much as Levaquin | Levofloxacin Tablet comes in category of low risk drug.
I am nursing mother and my doctor has suggested me to use Levaquin | Levofloxacin Tablet, is it safe?
Levaquin | Levofloxacin Tablet comes in category of low risk and if your doctor is aware that you are breastfeeding it should be ok to use without much concerns.
If I am using Levaquin | Levofloxacin Tablet, will my baby need extra monitoring?
Not much
Who can I talk to if I have questions about usage of Levaquin | Levofloxacin Tablet in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week