Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit while Breastfeeding
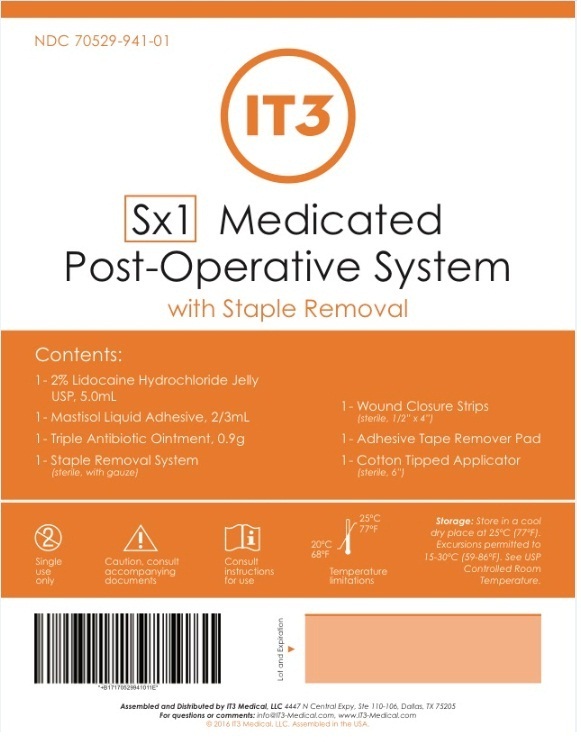
What is Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit used for?
Ask a doctor before use: First aid to help prevent infection in: Minor cuts scrapes burns
Brief: First aid to help prevent infection in: Minor cuts scrapes burns
Can I continue breastfeeding if I am using Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit? How long does it stays in breast milk?

Nursing Mothers: Lidocaine is secreted in human milk. The clinical significance of this observation is unknown. Caution should be exercised when lidocaine is administered to a nursing woman.
Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit Breastfeeding Analsys
Lidocaine hydrochloride anhydrous while Breastfeeding
SafeCAS Number: 137-58-6
Compatible with breastfeeding no matter the multiple ways it can be used: anesthetic, anti-arrhythmic, or anti-epileptic drug. Excreted into breast milk in non-significant amount with no side effects on breastfed infants from treated mothers. As a topical anesthetic (dermatologic, dental-stomatologic, ophtalmotologic and otologic preparations) it has an almost nil systemic absorption. Avoid using it on the nipple, but if necessary do it after the breast feed, wipe it out and rinse with water before the next feed, An euptectic mixture with added Prilocaine (EMLA) is used for dermatologic anesthesia. There is an increased risk of Methemoglobinemia when applied on large surfaces or taken by mouth. Intrapartum anesthesia may delay the onset of phase II of Lactogenesis or milk coming-in. The American Academy of Pediatrics rates it usually compatible with Breastfeeding.
Bacitracin while Breastfeeding
Safe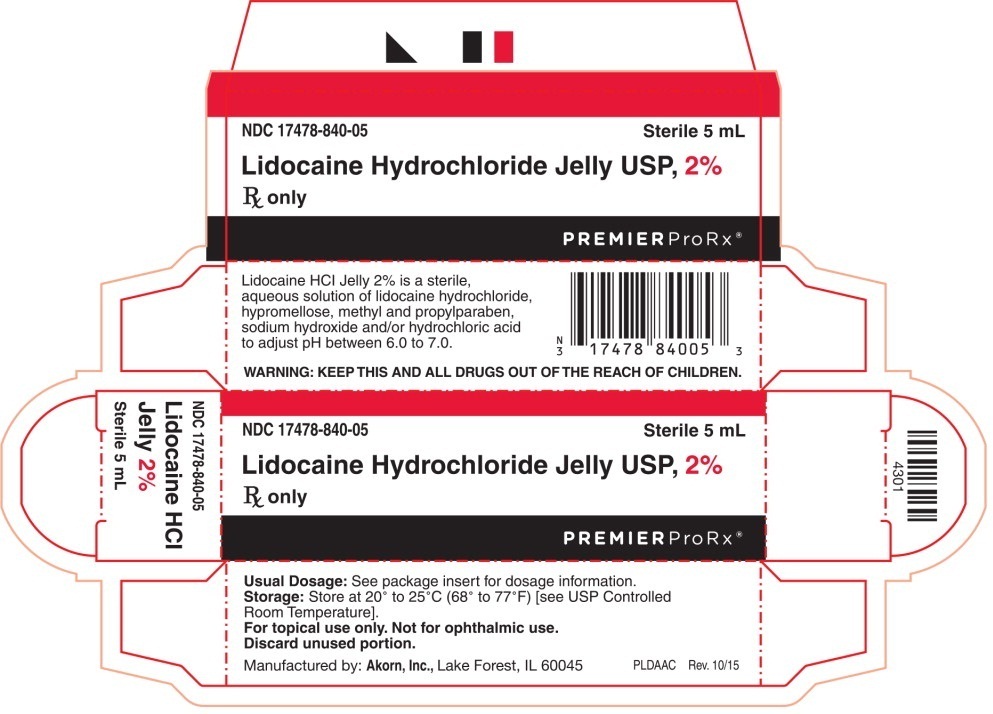
Polypeptide with anti-microbial activity that is produced by strains of Bacillus licheniformis or Bacillus subtilis. Indicated for topical use (high nephrotoxicity with systemic use) Not absorbed through skin, mucosa or intestinal tract. When orally taken it is destroyed by the gut with no pass into the blood stream. Preferably, avoid it on the breast or clear it out before nursing. Avoid use of creams, gels and other topical medication containing paraffin (petroleum-derived mineral oil) in order to avoid the risk of absorption by the child. The WHO Model List of Essential Medicines 2002 rates it as compatible with breastfeeding.
Neomycin while Breastfeeding
SafeCAS Number: 1404-04-2
Aminoglycoside antibiotic which is used in creams, eye drops, and otologic preparations for topical use, and, also orally used for intestinal disinfection. At latest update, relevant published data on excretion in the breast milk were not found. Like other aminoglycoside antibiotics, Neomycin is not absorbed by the gut. Absorption from other sources like skin, nose, ear and eye mucosa by means of topically used preparations (creams, drops, etc.) is very poor which causes excretion into breast milk in significant amount, unlikely. Do not apply creams, gels and other products that would contain paraffin (mineral oil) to avoid absorption by the infant since it is a hydrocarbon-derived substance. In case of use of Neomycin on the nipple, let it be done after the feed and wipe it out any excess of cream before the next feed. Be aware of false negative results of microbial cultures done from samples of febrile infants whose mothers are treated with antibiotics. Also, due to imbalance of intestinal flora a diarrheal disease can occur in the breastfed infant. List of Essential Medicines by WHO 2002: compatible with breastfeeding.
Polymyxin b while Breastfeeding
SafeCAS Number: 1405-20-5
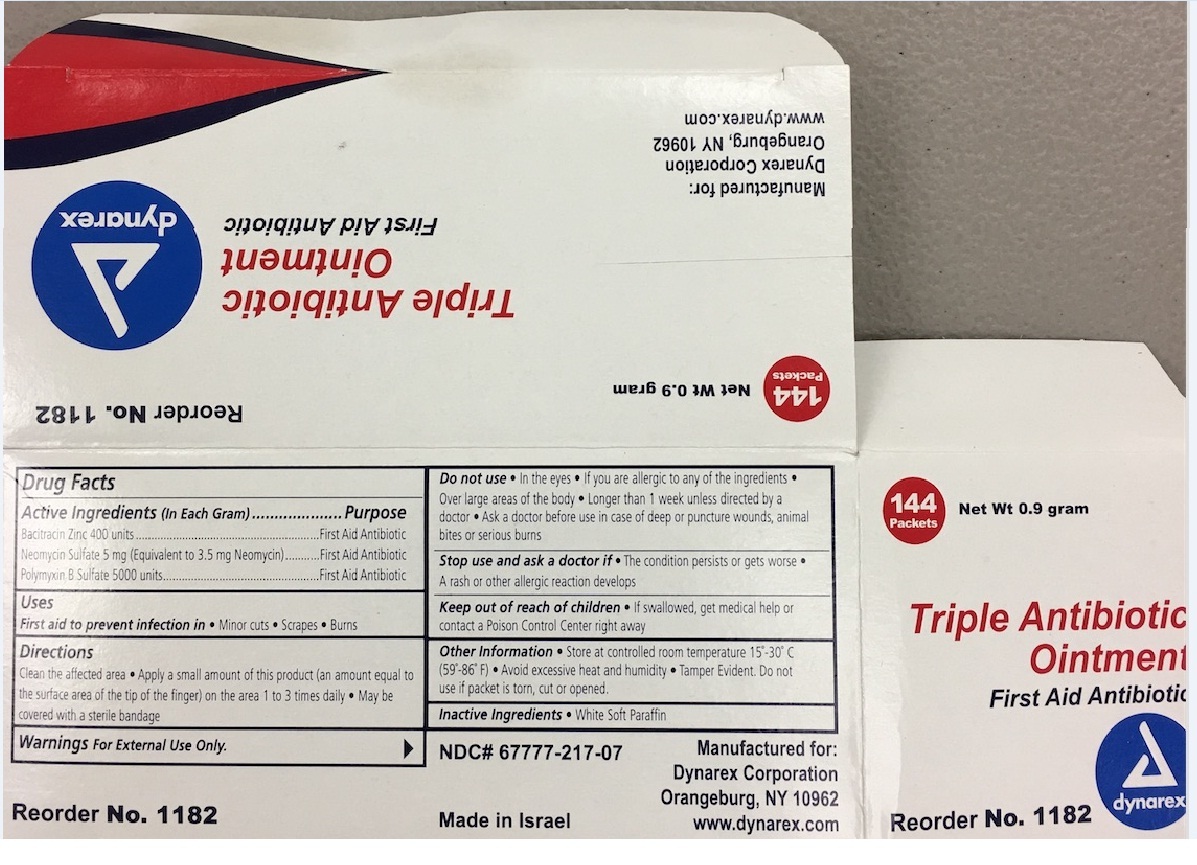
Antibiotic drug that is usual topically used (Dermatology, ENT and Ophthalmology) At latest update no published data on excretion into breast milk were found. The small dose and low absorption to the plasma in a majority of preparations that are topically used on the eye, ear or skin make a significant excretion into the milk unlikely. Its high molecular weight makes less probable an excretion into breast milk in significant amount. Due to a poor oral bioavailability, appearance in the infant's plasma from ingested milk is regarded as nil or scanty, except in premature infants or during the immediate neonatal period who may show an increased intestinal absorption. Polymyxin E or Colistin with a very similar molecular structure is excreted into breast milk in non-significant amount. It is advisable to avoid the application of creams, gels and other products for local use that would contain paraffin (mineral oil) to prevent absorption by the infant.
Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit Breastfeeding Analsys - 2
Lidocaine hydrochloride anhydrous while Breastfeeding
CAS Number: 137-58-6
Lidocaine concentrations in milk during continuous IV infusion, epidural administration and in high doses as a local anesthetic are low and the lidocaine is poorly absorbed by the infant. Lidocaine is not expected to cause any adverse effects in breastfed infants. No special precautions are required.[1][2][3] Lidocaine labor and delivery with other anesthetics and analgesics has been reported by some to interfere with breastfeeding. However, this assessment is controversial and complex because of the many different combinations of drugs, dosages and patient populations studied as well as the variety of techniques used and deficient design of many of the studies. Overall it appears that with good breastfeeding support epidural lidocaine with or without fentanyl or one of its derivatives has little or no adverse effect on breastfeeding success.[4][5][6][7][8] Labor pain medication may delay the onset of lactation.
Bacitracin while Breastfeeding
CAS Number: 1405-87-4
Because it is poorly absorbed after topical application and oral ingestion, bacitracin is considered a low risk to the nursing infant.[1] Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[2]
Neomycin while Breastfeeding
CAS Number: 1404-04-2
Although no information exists on the excretion of neomycin into milk, other aminoglycoside antibiotics are poorly excreted into breastmilk. Newborn infants apparently absorb small amounts of aminoglycosides, but serum levels are far below those attained when treating newborn infections and systemic effects of neomycin are unlikely. Older infants would be expected to absorb even less neomycin. Monitor the infant for possible effects on the gastrointestinal flora, such as diarrhea, candidiasis (e.g., thrush, diaper rash) or rarely, blood in the stool indicating possible antibiotic-associated colitis. Oral, topical, ophthalmic or otic neomycin should result in very low levels in breastmilk and present negligible risk to the infant,[1][2] although topical application to the nipple may increase the risk of diarrhea in the infant. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[3]
Polymyxin b while Breastfeeding
CAS Number: 1404-26-8
Because it is poorly absorbed after topical application, polymyxin B is considered a low risk to the nursing infant.[1] Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[2]
I already used Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit and meanwhile I breastfed my baby should I be concerned?
As usage of Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit is mostly safe while breastfeeding hence there should not be any concern. In case of any change in behavior or health of your baby you should inform your health care provider about usage of Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit else no further action is required.
My doctor has prescribed me Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit, what should I do?
Usage of Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit is safe for nursing mothers and baby, No worries.
If I am using Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit, will my baby need extra monitoring?
No
Who can I talk to if I have questions about usage of Sx1 Medicated Post-operative System | Lidocaine Hydrochloride Kit in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
