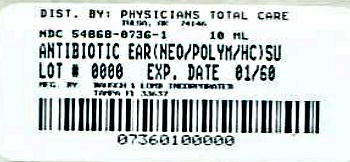
Antibiotic Ear (neo/polym/hc) while Breastfeeding
What is Antibiotic Ear (neo/polym/hc) used for?
I am breastfeeding mother and I am using Antibiotic Ear (neo/polym/hc). Can it have any bad effect on my kid? Shall I search for better alternative?

Nursing Mothers: Hydrocortisone appears in human milk following oral administration of the drug. Since systemic absorption of hydrocortisone may occur when applied topically, caution should be exercised when neomycin and polymyxin B sulfates and hydrocortisone otic solution is used by a nursing woman.
Antibiotic Ear (neo/polym/hc) Breastfeeding Analsys
Neomycin while Breastfeeding
SafeCAS Number: 1404-04-2
Aminoglycoside antibiotic which is used in creams, eye drops, and otologic preparations for topical use, and, also orally used for intestinal disinfection. At latest update, relevant published data on excretion in the breast milk were not found. Like other aminoglycoside antibiotics, Neomycin is not absorbed by the gut. Absorption from other sources like skin, nose, ear and eye mucosa by means of topically used preparations (creams, drops, etc.) is very poor which causes excretion into breast milk in significant amount, unlikely. Do not apply creams, gels and other products that would contain paraffin (mineral oil) to avoid absorption by the infant since it is a hydrocarbon-derived substance. In case of use of Neomycin on the nipple, let it be done after the feed and wipe it out any excess of cream before the next feed. Be aware of false negative results of microbial cultures done from samples of febrile infants whose mothers are treated with antibiotics. Also, due to imbalance of intestinal flora a diarrheal disease can occur in the breastfed infant. List of Essential Medicines by WHO 2002: compatible with breastfeeding.
Polymyxin b while Breastfeeding
SafeCAS Number: 1405-20-5
Antibiotic drug that is usual topically used (Dermatology, ENT and Ophthalmology) At latest update no published data on excretion into breast milk were found. The small dose and low absorption to the plasma in a majority of preparations that are topically used on the eye, ear or skin make a significant excretion into the milk unlikely. Its high molecular weight makes less probable an excretion into breast milk in significant amount. Due to a poor oral bioavailability, appearance in the infant's plasma from ingested milk is regarded as nil or scanty, except in premature infants or during the immediate neonatal period who may show an increased intestinal absorption. Polymyxin E or Colistin with a very similar molecular structure is excreted into breast milk in non-significant amount. It is advisable to avoid the application of creams, gels and other products for local use that would contain paraffin (mineral oil) to prevent absorption by the infant.
Hydrocortisone while Breastfeeding
SafeCAS Number: 50-23-7
Cortisol is a normal component of breast milk. Although unlikely to achieve harmful levels for the infant, it is preferred the use of an alternative (Methylprednisolone, Prednisolone, Prednisone). Intra-articular administration of depot prednisone derivatives may be a cause of transient decrease of milk production. Eleventh WHO Model List of Essential Drugs 2002: Compatible with breastfeeding.
Antibiotic Ear (neo/polym/hc) Breastfeeding Analsys - 2
Neomycin while Breastfeeding
CAS Number: 1404-04-2
Although no information exists on the excretion of neomycin into milk, other aminoglycoside antibiotics are poorly excreted into breastmilk. Newborn infants apparently absorb small amounts of aminoglycosides, but serum levels are far below those attained when treating newborn infections and systemic effects of neomycin are unlikely. Older infants would be expected to absorb even less neomycin. Monitor the infant for possible effects on the gastrointestinal flora, such as diarrhea, candidiasis (e.g., thrush, diaper rash) or rarely, blood in the stool indicating possible antibiotic-associated colitis. Oral, topical, ophthalmic or otic neomycin should result in very low levels in breastmilk and present negligible risk to the infant,[1][2] although topical application to the nipple may increase the risk of diarrhea in the infant. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[3]
Polymyxin b while Breastfeeding
CAS Number: 1404-26-8
Because it is poorly absorbed after topical application, polymyxin B is considered a low risk to the nursing infant.[1] Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[2]
Hydrocortisone while Breastfeeding
CAS Number: 50-23-7
Hydrocortisone (cortisol) is a normal component of breastmilk that passes from the mother's bloodstream into milk and might have a role in intestinal maturation, the intestinal microbiome, growth, body composition or neurodevelopment, but adequate studies are lacking.[1] Concentrations follow a diurnal rhythm, with the highest concentrations in the morning at about 7:00 am and the lowest concentrations in the late afternoon and evening.[2][3] Cortisol in milk may protect against later infant obesity, especially in girls.[4] Hydrocortisone has not been studied in breastmilk after exogenous administration in pharmacologic amounts. Hydrocortisone in breastmilk is stable at room temperature and during repeated freeze-thaw cycles.[5] Although it is unlikely that dangerous amounts of hydrocortisone would reach the infant, a better studied alternate corticosteroid might be preferred. Maternal use of hydrocortisone as an enema would not be expected to cause any adverse effects in breastfed infants. Local maternal injections, such as for tendinitis, would not be expected to cause any adverse effects in breastfed infants, but might occasionally cause temporary loss of milk supply. See also Hydrocortisone, Topical. Hydrocortisone concentrations in breastmilk are not affected by storage for 36 hours at room temperature, during multiple freeze-thaw cycles, nor Holder pasteurization (62.5 degrees C for 30 minutes).[5][6]
What if I already have used Antibiotic Ear (neo/polym/hc)?
Antibiotic Ear (neo/polym/hc) is safe in breastfeeding and should not create any health problem for your baby but in case you feel any health issue associated with Antibiotic Ear (neo/polym/hc) you should contact your doctor or health care provider. Be it pregnancy or lactation you shall keep your doctor informed.
I am nursing mother and my doctor has suggested me to use Antibiotic Ear (neo/polym/hc), is it safe?
Usage of Antibiotic Ear (neo/polym/hc) is safe for nursing mothers and baby, No worries.
If I am using Antibiotic Ear (neo/polym/hc), will my baby need extra monitoring?
No
Who can I talk to if I have questions about usage of Antibiotic Ear (neo/polym/hc) in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
