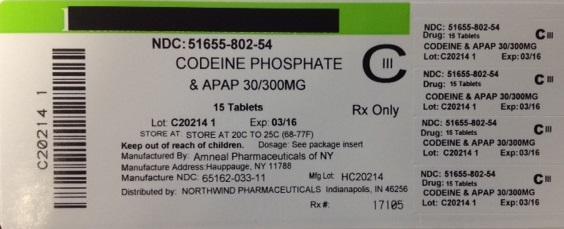
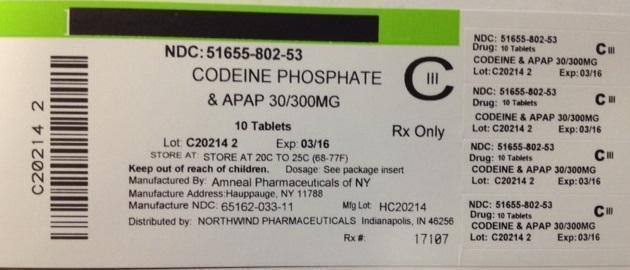
Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet while Breastfeeding
What is Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet used for?
Can I continue breastfeeding if I am using Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet? How long does it stays in breast milk?

Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet Breastfeeding Analsys
Acetaminophen while Breastfeeding
SafeCAS Number: 103-90-2
Excreted in very low amount into breast milk. Infant intake may be lower than 4% of usual pediatric dose. The American Academy of Pediatrics rates it as compatible with Breastfeeding.
Codeine phosphate while Breastfeeding
UnsafeCAS Number: 76-57-3
Compound of cough and pain medication. The cytochrome P450-CYP2D6 enzyme catalyzes morphine. It is excreted in breast milk in small amounts, much lower than the dose used for newborns and infants. The plasma levels of infants whose mothers take them are very low, less than usual therapeutic levels and assuming an insignificant relative dose, less than 1.5% (Meny 1993, Naumburg 1988, Findlay 1981), so it was considered safe for use during breastfeeding (Bar-Oz 2003, WHO 2002, AAP 2001, Moretti 2000, Spigset 2000, Mitchell 1999, Meny 1993). However, excessive sedation in the mother or infant may occur if they are rapid metabolizers of codeine to morphine due to an excess of the gene linked to the P450-2D6 enzyme: this occurs in <1% of Chinese, Japanese and Hispanic people; 3% African Americans; 1-10% of Caucasians and 16-29% of North Africans, Ethiopians and Saudis (Halder 2015, Sachs 2013). The genetic diagnosis of this characteristic is not available in usual clinical practice (Madadi, 2011). Codeine through breast milk has been linked to the appearance of neonatal apnea (Naumburg, 1988), drowsiness (Ito, 1993), neurological depression (Madadi, 2008) and, above all, a fatal outcome: a newborn whose mother had this genetic abnormality died at 13 days; the mother was taking 60 mg of codeine twice daily, morphine levels were normal in breast milk, but very high in the child's plasma (Madadi 2007, Koren 2006). Subsequently, the causality of codeine in this case has been called into question (Bateman 2008, Ferner RE 2008, Young 2007). A link has been found between the use of codeine during pregnancy and breastfeeding and the risk of developing neuroblastoma in the infant (Cook, 2004). Because of all this, and with newborns having a limited capacity for opioid elimination (Willmann, 2009) and the existence of more effective alternatives, many authors and institutions advocate completely discouraging its use in infants and breastfeeding mothers (FDA 2017, Al-Adhami 2016, Lazaryan 2015, AEMPS 2015, Sachs 2013, EMA 2013). Other authors advocate cautious use (some even in the case of rapid metabolizers), using the lowest possible effective dose and for no more than 4 days and monitoring for signs of sedation in mother and infant (Royal Berkshire-NHS 2016, Halder 2015, Reece-Stremtan-ABM Protocol#21 2015, Chow 2015, Kelly 2013, UKMi NHS 2013, Rowe 2013, Montgomery-ABM protocol#15 2012, Amir 2011, Madadi 2009, Madadi 2007, FDA 2007). The use of non-steroidal anti-inflammatory drugs (NSAIDs) better controls pain and with fewer side effects than codeine alone or in combination with paracetamol (Palanisamy 2014, Hendrickson 2012, van den Anker 2012, Madadi 2009, Nauta 2009, Willmann 2009), and codeine is not included either in international consensus on the treatment of migraines (Bordini 2016, Worthington 2013). Follow WHO standards for childbirth attendance, reduce cesarean sections and episiotomies, and therefore the need for analgesics in the first few days.
Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet Breastfeeding Analsys - 2
Acetaminophen while Breastfeeding
CAS Number: 103-90-2
Acetaminophen is a good choice for analgesia, and fever reduction in nursing mothers. Amounts in milk are much less than doses usually given to infants. Adverse effects in breastfed infants appear to be rare.
Codeine phosphate while Breastfeeding
CAS Number: 76-57-3
Maternal use of codeine during breastfeeding can cause infant drowsiness, central nervous system depression and even death, with pharmacogenetics possibly playing a role.[1][2] Newborn infants seem to be particularly sensitive to the effects of even small dosages of narcotic analgesics. Once the mother's milk comes in, it is best to provide pain control with a nonnarcotic analgesic and limit maternal intake of oral codeine to 2-4 days at a low dosage with close infant monitoring, especially in the outpatient setting.[2][3][4][5] If the baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness, a physician should be contacted immediately.[6] Excessive sedation in the mother often correlates with excess sedation in the breastfed infant. Following these precautions can lower the risk of neonatal sedation.[7] Numerous professional organizations and regulatory agencies recommend that other agents are preferred over codeine or to avoid codeine completely during breastfeeding;[8][9][10][11][12] however, other opioid alternatives have been studied less and may not be safer.[13]
I already used Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet and meanwhile I breastfed my baby should I be concerned?
We have already established that Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet is unsafe in breastfeeding and breastfeeding while using Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet is not a good idea however if have already used
My doctor has prescribed me Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet, what should I do?
If your doctor knows that you are breastfeeding mother and still prescribes Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet then there must be good reason for that as Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet is considered unsafe, It usually happens when doctor finds that overall advantage of taking
If I am using Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet, will my baby need extra monitoring?
Yes, Extra monitoring is required if mother is using Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet and breastfeeding as it is considered unsafe for baby.
Who can I talk to if I have questions about usage of Acetaminophen And Codeine | Codeine Phosphate And Apap Tablet in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
